WorkSafe 3: Investigation into Victorian self-insurers’ claims management and WorkSafe oversight
Date posted:Foreword
They helped me transition to a new position and get the treatment I needed.
Comment from injured worker
They took months to start my payment and have made many mistakes with my weekly payments causing a huge amount of stress in an already stressful period.
Comment from injured worker
This is my third report into Victoria’s workers compensation scheme. It concerns an area I did not look at in my two previous reports; what happens when companies are authorised by WorkSafe to handle their own claims, rather than using a WorkSafe-appointed agent.
My previous reports were highly critical of agent practices and WorkSafe’s oversight of them, and have resulted in significant reforms, which I welcome. But many people expressed concerns that those reforms did not extend to companies acting as self-insurers. Did the same problems exist? Is it appropriate for those reforms to be extended? This investigation seeks to answer those questions.
There is an obvious power imbalance between injured workers and their employer, which can be exacerbated where the employer is also their insurer. On the other hand, when an employer offers tailored rehabilitative support, this relationship can also be an advantage.
Thirty-four companies – covering about 120,000 Victorian workers and including many of Victoria’s largest employers – are currently approved to manage their own claims. The number and scale of companies acting as self-insurers imposed some challenges on the investigation; it was simply not practicable to fully explore the decision-making practices of each. We therefore focused on complaints, but acknowledge that self-insurers manage many claims and most are handled without complaint.
We found some self-insurers performing well and delivering the benefits the system intends. But the cases we examined in detail exposed large differences in both practice and capability. It was apparent that self-insurers’ claims management processes did not always produce fair outcomes for workers, and that some echoed the undesirable practices used by WorkSafe agents that my two previous reports exposed.
Given the wide variance of practices across 34 companies, we focused on the role of WorkSafe, which is responsible for approving and monitoring self-insurers to enforce performance standards and promote good decision-making.
Ultimately, we found that more needs to be done – by WorkSafe, to ensure its oversight role is meaningful, and by government, to ensure greater consistency for workers.
We found multiple lost opportunities in WorkSafe’s oversight, including a reluctance to become involved when self-insurers make unsustainable decisions and to use its approval power to support compliance.
WorkSafe has fewer levers for dealing with self-insurers than for agents. In particular, it has no power to direct a self-insurer to overturn a decision. However, WorkSafe seemed unwilling to use the levers it has. We were troubled by WorkSafe’s tendency to use its discretion to approve the maximum six-year term for self-insurers with claims management performance issues. There is also little transparency regarding self-insurers, with WorkSafe publishing little information about their performance.
The picture we saw was not of a broken system, but a patchy and unequal one. Workers should not have a fundamentally different claims experience depending on who their employer is. All self-insurers are equally bound by legislation to ensure that compensation ‘is paid to injured workers in the most socially and economically appropriate manner, as expeditiously as possible’.
I am pleased that WorkSafe acknowledges it needs to do more and is committing to greater vigilance in its regulatory oversight. Reviews and assessment should be purposeful and result in timely regulatory action; ensuring fair outcomes are achieved and decisions are made that are compatible with human rights.
I said in my first WorkSafe report, in 2016, that workers compensation has a fraught history; successive governments have wrestled with the complexity of creating a scheme that is both financially viable and fair. I acknowledge that the government continues to do so. The modest reforms proposed here should increase fairness – for example, by giving WorkSafe the power to direct self-insurers – without affecting financial viability.
The government and WorkSafe have responded admirably to my previous recommendations to ensure a fairer, more equitable system – for the sake of the next generation of injured workers and the community that bears the cost. It is in everyone’s interests to promote sustainable and timely decision-making on what are not merely numbers, files or claims, but people’s lives and livelihoods.
Until all workers in Victoria with the right to claim compensation have the same rights when they disagree with a decision, the system will not be truly fair.
We will continue to monitor both the successes and gaps in the system through the complaints made to us, and this report exposes the gaps around self-insurers. It has been a long journey to systemic fairness, and we are not there yet.
Deborah Glass
Glossary
| Arbitration | A process in which a binding decision is made in relation to a dispute. Arbitration is sought when a dispute has not been settled at conciliation. |
| Case Manager | Primary contact for both the employee and employer. The Case Manager's primary role is to manage a portfolio of claims by coordinating the treatment and recovery of injured workers. |
| Claimant | An injured worker who makes a workers compensation claim. |
| Conciliation | A dispute resolution process that brings the people involved in a disputed claim together to try to achieve an agreement. The people involved include the injured worker, the self-insurer and/or their agent. |
| IME | Independent Medical Examiner. An IME is a registered health practitioner approved by Worksafe to undertake a medical examination under the WIRC Act. |
| Injured worker | Independent Medical Examiner. An IME is a registered health practitioner approved by Worksafe to undertake a medical examination under the WIRC Act. |
| Medical Panel | An expert panel tasked with providing legally binding answers to medical questions that assists in resolving disputes. |
| Non-compliance | Under WorkSafe’s Self-audit Tool, a failure to meet a workers compensation legislative requirement. |
| Prompted satisfaction | A category of response in an injured worker survey: the response of an injured worker to a question about overall satisfaction asked after other questions about specific aspects of service. |
| Self-insurer | A company (‘body corporate’) approved by WorkSafe under legislation, to manage and fund the workers compensation claims of their employees instead of paying premiums to WorkSafe. |
| Substantiated complaint | Defined by WorkSafe as a complaint where it finds some evidence of a potential breach of the WIRC Act. |
| Unsustainable decision | A decision that does not have a reasonable prospect of withstanding a court challenge. |
| WCIRS | The Workers Compensation Independent Review Service. An independent review team within Worksafe that provides injured workers with a review of some Agent and WorkSafe decisions. Injured workers of self-insurers cannot currently request a review from this team. |
| WIC | When a WIC Conciliation Officer is unable to bring the parties to agreement and considers there to be an arguable case on the part of the self-insurer or their agent. A genuine dispute certificate allows the matter to proceed to arbitration or court. |
| WIC – genuine dispute | When a WIC Conciliation Officer is unable to bring the parties to agreement and considers there to be an arguable case on the part of the self-insurer or their agent. A genuine dispute certificate allows the matter to proceed to arbitration or court. |
| WIC – Direction | When a WIC Conciliation Officer deems that an self-insurer or their agent has no arguable case to deny liability to pay weekly compensation or medical and like expenses to a worker they may direct that limited payments are made. |
| WIRC Act | Workplace Injury Rehabilitation and Compensation Act 2013 (Vic) |
| Workers compensation | A payment to employees injured at work or who become sick as a result of their work. It includes payments to employees to cover their wages while they are not fit for work, medical expenses and rehabilitation. |
| WorkSafe | The trading name for the Victorian Workcover Authority, a statutory authority of the Victorian government created under the Accident Compensation Act 1985 (Vic). |
Background
1. Victoria’s statutory workers compensation scheme enables eligible injured workers to claim compensation and receive support to help them recover and, where possible, return to work.
2. The Workplace Injury Rehabilitation and Compensation Act 2013 (Vic) (‘WIRC Act’) outlines a range of entitlements under the scheme, including weekly income payments for those unable to work, and payments to cover reasonable treatment costs.
3. One of the objectives of the WIRC Act is that compensation ‘is paid to injured workers in the most socially and economically appropriate manner, as expeditiously as possible’.
4. The scheme is managed by the Victorian WorkCover Authority (‘WorkSafe’), and operates on a ‘no fault’ basis, meaning employees are covered if they are injured at work, regardless of who is at fault.
5. The scheme is largely funded by compulsory annual insurance premiums paid by employers. In return, WorkSafe takes on liability for most workers compensation claims, outsourcing them to private agents to manage. Four WorkSafe agents in Victoria manage all the claims for about 95 per cent of the cost of the scheme.
6. The WIRC Act also allows for some eligible employers, mostly larger corporations, to run their own separate claims process instead of paying compulsory premiums to WorkSafe. These employers are known as ‘self-insurers’.
7. There are 34 approved self-insurers at the time of writing, covering about 120,000 Victorian workers and including many of Victoria’s largest employers (see full list in Appendix 2).
8. Most self-insurers handle claims in-house; but just as WorkSafe uses private agents to manage claims, some self-insurers also outsource claims management to private agents. Eight self-insurers have WorkSafe approval to outsource the management of some or all of their claims to agents.
9. WorkSafe is responsible for approving and monitoring self-insurers (and their agents) to enforce performance standards and promote good decision-making.
Our prior WorkSafe investigations
10. This is the Ombudsman’s third investigation into the administration of Victoria’s statutory workers compensation scheme. The first two were confined to WorkSafe and its agents, and did not look at self-insurers.
11. Our first report in 2016 looked at how WorkSafe’s agents handled difficult and expensive compensation claims, and WorkSafe’s oversight of them. The report concluded while the system was not broken, the handling of complex claims needed reform. WorkSafe accepted all 15 Ombudsman recommendations, with the support of the responsible Minister.
12. However, over the next few years we continued to receive complaints and heard anecdotal evidence not enough had changed.
13. Our second report in 2019 found some WorkSafe agents were continuing to make unreasonable decisions, leaving workers stuck in time-consuming, stressful and costly disputes. It was evident more systemic reform was needed.
14. We made three key recommendations. First, that the Victorian Government review whether the WorkSafe agent model remained appropriate for complex claims. In response, the Government commissioned Improving the experience of injured workers: A review of WorkSafe Victoria’s management of complex workers compensation claims (‘the Rozen report’), published in April 2021.
15. Second, the Ombudsman recommended the Government address a shortcoming in the dispute resolution system – that only a lengthy and costly court process could deliver a binding outcome where other efforts to resolve a dispute, such as conciliation, had failed.
16. In response, the Government introduced legislation allowing arbitration as an option for injured workers after conciliation. All Victorian workers, including those working for self-insurers, can now seek binding determinations on disputes without having to go to court.
17. Third, the Ombudsman recommended WorkSafe establish a dedicated business unit to independently review disputed decisions following unsuccessful conciliation, and use its existing powers to direct its agents to overturn decisions unlikely to be upheld if challenged in court.
18. In response, the Workers Compensation Independent Review Service (‘WCIRS’) began in 2020. WorkSafe says in its first three years, WCIRS has had a significant impact, with fewer adverse decisions needing to be overturned, suggesting a measurable improvement in the quality of WorkSafe agent decision-making. It is hoped that more injured workers are getting timely and fair outcomes because of this change.
19. However, not all Victorian workers can take their concerns to WCIRS, with injured workers of self-insurers being excluded from using the service.
Figure 1: Victoria’s workers compensation system
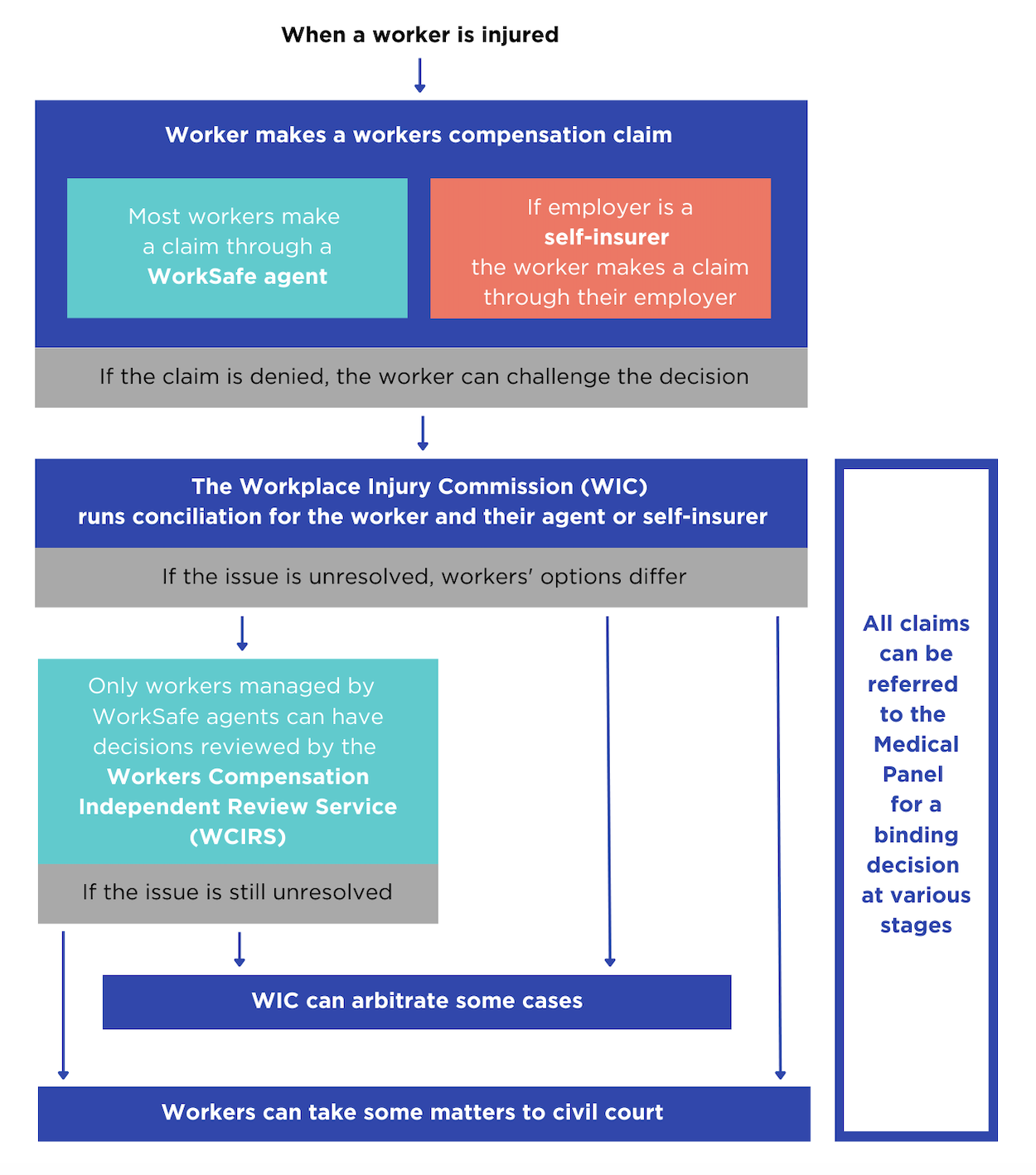
Source: Victorian Ombudsman
Why we investigated
20. Following the Ombudsman’s two WorkSafe investigations, we continued to receive complaints from injured workers of self-insurers. Those complaints often echoed those made about WorkSafe agents. People complained about self-insurers making unreasonable claims decisions not supported by evidence.
21. Unions and other stakeholders have criticised the self-insurer scheme. Some criticisms are about the conduct of individual companies, including the use of technical grounds to deny claims, the misuse of medical evidence and a litigious approach to conciliation.
22. WorkSafe’s annual surveys of injured workers from at least 2018 onward consistently show self-insurer workers are about 10 per cent less satisfied than those with claims managed by WorkSafe agents.
23. We received data from the Workplace Injury Commission (‘WIC’). WIC is an independent authority established under the WIRC Act to help resolve workplace compensation disputes. WIC data for the 2020-21 and 2021-22 financial years showed notably lower rates of resolution at conciliation where a self-insurer was involved.
24. WIC told the investigation it had observed positive changes in WorkSafe agent decision-making after the Ombudsman’s second WorkSafe report but this had not flowed through to some self-insurer decision-making. WIC stated some self-insurers were not meaningfully engaging in the conciliation process and were continuing to dispute matters unlikely to be upheld if challenged in court (‘unsustainable decisions’). WIC suggested a lack of improvement by self-insurers in these areas may have been due, in part, to the limits of WorkSafe’s role as regulator.
25. WIC noted injured workers of self-insurers were unable to seek a WCIRS review of a decision. This gap was highlighted by many when we called for public submissions to our investigation, and by the Rozen review. WCIRS cannot review decisions made by or on behalf of a self-insurer, because WorkSafe has no power to direct self-insurers to overturn decisions. This places workers of self-insurers at a disadvantage compared to most Victorian workers.
26. Another theme in complaints to the Ombudsman and submissions to the investigation was WorkSafe’s oversight of self-insurers, and whether it can or does effectively address issues. Half of the 22 submissions that informed the Rozen review highlighted that self-insurers were engaging in the same practices WorkSafe agents had been prior to the Ombudsman’s investigations. In response to these concerns, WorkSafe stated that it was implementing changes to align the review of self-insurer decision-making with that of WorkSafe agents. WorkSafe stated it was not taking any specific action to agitate for the power to overturn self-insurer decisions in response to the Rozen report.
27. Based on all of this – public complaints and submissions to the Ombudsman, the Rozen review and WorkSafe’s response to its report, information from WIC and WorkSafe’s surveys of injured workers – the Ombudsman decided to investigate.
Figure 2: Voices of injured workers
Workers’ experiences with self-insurers varied significantly. These quotes from injured worker surveys describe both positive and negative encounters.


The investigation
28. On 27 May 2022, the Ombudsman notified the relevant Minister, Chief Executive Officer of WorkSafe, Chair of WorkSafe’s Board of Directors and the Chief Executive Officer of the Accident Compensation Conciliation Service (now WIC) of her intention to conduct an ‘own motion’ investigation, under 16A of the Ombudsman Act 1973 (Vic), into self-insurers’ claims management and WorkSafe’s oversight.
29. Between 27 and 30 May 2022, the Ombudsman also notified the Principal Officer of each of Victoria’s 34 self-insurers.
30. On 14 July 2022 the Ombudsman publicly announced her decision to conduct the investigation and called for public submissions.
31. The objective of the investigation was to establish whether the claims management processes of self-insurers provide fair and equitable outcomes for their injured workers and whether the oversight processes of WorkSafe contribute to fair and equitable outcomes for injured workers of self-insurers.
32. Although self-insurers are required to manage claims in accordance with the WIRC Act and adopt the same claims management practices as WorkSafe agents, they have a discretion to take different approaches. The case studies and practice notes in this report highlight only a slice of the varying claims management approaches taken by self-insurers. They are included to encourage all self-insurers and WorkSafe to reflect on industry standards, and whether the current system is delivering fair outcomes and preserving workers’ rights under the Act. Specific self-insurers are not identified in these samples to protect the privacy of the injured workers.
How we investigated
33. The investigation received 45 submissions, including from seven self-insurers, an agent who represented three self-insurers, injured workers and their advocates, lawyers, industry groups, unions and health care providers. Through submissions and other sources, about 240 claim files were identified for possible examination; and 87 of these were obtained from self-insurers and reviewed in detail. Information was also sought from WorkSafe and WIC, and we spoke to 20 injured workers and their advocates.
34. In all, the investigation obtained more than 850,000 documents, and reviewed material including:
- selected self-insurer files and correspondence
- data about the outcomes of disputed claims
- examples provided by self-insurers at our request demonstrating best practice
- WorkSafe documents, including processes, guidelines and assessments of self-insurer performance
- WIC data, files, and feedback about the participation of self-insurers at conciliation.

35. Further details about what the investigation examined are included in Appendix 1.
Procedural fairness and privacy
36. The investigation is guided by the civil standard of proof, the balance of probabilities, in determining the facts of the investigation – taking into consideration the nature and seriousness of the matters examined, the quality of the evidence, and the gravity of the consequences that may result from any adverse opinion.
37. This report includes adverse comments about WorkSafe as the regulator of self-insurers. While the Ombudsman has not made adverse comments or conclusions about specific self-insurers, or their agents, it does include data, practice examples and comments from third parties, including injured workers, about claims management that may be perceived as adverse to self-insurers.
38. In accordance with section 25A(2) of the Ombudsman Act, the investigation has provided WorkSafe, each of the 34 self-insurers, and two agents who act for self-insurers, with a reasonable opportunity to respond to the material in the report. This report fairly sets out their responses.
39. Relevant excerpts of a draft of this report (‘the draft report’) were provided to the injured workers whose stories are detailed in de-identified case studies and to WIC, to confirm factual accuracy. Self-insurers were also provided with excerpts of the case studies to confirm factual accuracy. This report fairly reflects their responses.
40. In accordance with section 25A(3) of the Ombudsman Act, any other persons or bodies who are or may be identifiable from the information in this report are not the subject of any adverse comment or opinion. They are named or identified in the report as the Ombudsman is satisfied that:
- it is necessary or desirable to do so in the public interest
- identifying those persons will not cause unreasonable damage to those persons’ reputation, safety or wellbeing.
41. To protect the privacy and welfare of injured workers, case studies in the report exclude identifying details such as employer names and dates. All case studies relate to claims made between 2016 and 2022.
42. In response to the draft report, some self-insurers provided detailed responses to specific points which are incorporated in the final report. The names of self-insurers are used in these instances as they do not identify individual workers.
43. It should not be inferred that claims management practices or decisions made on an individual case highlighted in this report reflect a self-insurer’s or their agent’s approach or performance in other cases. Some self-insurers manage many claims, and most are handled without complaint or necessary intervention from WorkSafe.
44. Nevertheless, it is important that injured workers’ stories are heard, and their experiences valued and understood. From the 87 workers’ stories examined in detail, the case studies we have included were chosen to reflect questionable or problematic claims management practices, and their adverse impacts. Some case studies were removed from the final report at the request of the injured workers who said they were still affected by the management of their claim, or were fearful of reprisals.
45. Any of us can be injured at work, and we are all entitled to expect best practice in response. All self-insurers and their agents can learn from the case studies and practice examples in this report. Adherence to best practice leads to appropriate compensation as intended by the WIRC Act.
About the self-insurer scheme
46. WorkSafe’s website states the role of self-insurance in Victoria is to ‘provide choice to eligible employers to manage and bear the costs and risks of their own claims’. WorkSafe advises self-insurance should:
- provide direct incentives to improve injury prevention and rehabilitation performance
- ensure that workers are treated fairly and equitably
- contribute to continuous improvement in health and safety and return to work performance.
47. In the financial year ending June 2022, 1,713 claims were lodged with self-insurers. Unlike some of its interstate counterparts, WorkSafe does not publish claim numbers or statistics, however WorkSafe advised the investigation that self-insurers were managing 3,032 active claims at the end of December 2022.
48. WorkSafe is responsible for approving self-insurers under the WIRC Act. WorkSafe first determines if the company is eligible. This includes whether the company has the financial viability to meet its claims liabilities.
49. To be satisfied that a company is ‘fit and proper’ to be a self-insurer, WorkSafe must also consider:
- the safety of working conditions at the company
- the number of workplace injuries
- the cost of associated claims
- the resources, including employees, the company has to administer compensation claims.
50. WorkSafe’s oversight framework is based on the WIRC Act and associated Ministerial Orders and WorkSafe Guidelines. WorkSafe regulates self-insurers using:
- a ‘tier’ system
- the Self-insurer Self-audit Program
- a Regulatory Claims Audit Program
- post-audit performance improvement plans
- monitoring and reporting systems.
51. WorkSafe also conducts Quality Decision Making Audits (‘Quality Decision Audits’) of both WorkSafe agent and self-insurer decisions. A sample of claims decisions are reviewed every year to confirm alignment with good decision-making principles and the law. The audits focus on compliance with WorkSafe’s Claims Manual and Quality Ethical Decision-Making Guidelines.
52. The Quality Decision Audits consider whether reasonable and appropriate evidence was sought and considered, whether the decision was correct in the circumstances, and whether it was ‘sustainable’. Decisions are considered unsustainable if they do not have a reasonable prospect of withstanding a court challenge.
53. When there is a dispute about a claim, the matter can be conciliated through WIC. This is true regardless of whether a WorkSafe agent or a self-insurer is managing the claim.
54. WIC is an independent authority responsible to the Minister for WorkSafe and the TAC and reports through the Department of Treasury and Finance.
55. WIC’s website states conciliation gives an injured worker ‘the opportunity to come together with others involved in a workplace compensation dispute to find a way forward as quickly as possible’.
56. The goal of conciliation is to resolve disputes by involving all parties in an informal, non-adversarial process to reach a fair and mutually acceptable agreement. Ministerial Guidelines govern the conduct of self-insurers and employee representatives during the conciliation process.
57. In 2021-22, workers referred 9,182 disputes in total to WIC for conciliation, with resolution rates of 69 per cent for WorkSafe agents and 58 per cent for self-insurers (and their agents).
58. Where a matter cannot be resolved, Conciliation Officers have the power to:
- dismiss the dispute
- make recommendations
- refer medical questions to a Medical Panel
- issue a ‘genuine dispute certificate’.
59. A genuine dispute certificate is needed before the parties can take the matter to arbitration or court. In limited circumstances, Conciliation Officers also have the power to give a Direction to a WorkSafe agent or a self-insurer to make payments to the worker.
60. Some disputes are referred to a Medical Panel for a determination on medical questions. Medical Panels can be used by WIC or a court to resolve a dispute where there are medical questions regarding a worker’s injuries. These questions may relate to diagnosis, causation, work capacity or the appropriateness of treatment.
61. Each Medical Panel is independent and made up of expert specialist doctors. The Panel functions as a tribunal that provides final and legally binding answers to the medical questions referred to it.
62. In 2021-22, WIC referred 1,151 matters to Medical Panels. About 14 per cent (163) of these were for claims involving self-insurers.
63. If conciliation is unsuccessful and a genuine dispute certificate issued, injured workers now have two potential options.
64. Until recently their only choice was to go to court. Workers injured on or after 1 September 2022 now have an option for the matter to be arbitrated by WIC under the Workplace Injury Rehabilitation and Compensation Amendment (Arbitration) Act 2021 (Vic).
65. This is a welcome system improvement, however, not all disputes are eligible for arbitration.
66. Arbitration can only provide a final decision on compensation disputes involving weekly payments, medical expenses, superannuation contributions and interest on an outstanding amount. In other cases, the worker’s only option remains court.
67. As the regulator, WorkSafe has a role to support self-insurers to understand their obligations under the Charter of Human Rights and Responsibilities Act 2006 (Vic) (‘Charter of Rights Act’).
68. This Act protects basic rights and freedoms of Victorians, such as the right to privacy and reputation. It promotes a culture where human rights are protected and considered in service delivery, policy, decisions, and legislation.
69. Under the Charter of Rights Act, it is generally unlawful for public authorities to:
- act in a way that is incompatible with a human right; or
- fail to give proper consideration to a relevant human right when making a decision.
70. Public statutory bodies, like WorkSafe, must act compatibly with, and give proper consideration to, relevant human rights when making decisions. Self-insurers, when licensed by WorkSafe to perform functions under the WIRC Act, are also required to consider these rights. The Charter of Rights Act recognises that human rights are not absolute and may be limited but any limitation must be reasonable and justified.
Self-insurers’ claims management
71. In Victoria, self-insurer decision-making on claims must be guided by the WIRC Act and the WorkSafe Claims Manual, which sets out principles of good administrative decision-making. Although it is permitted for Victorian self-insurers to create their own claims management policies, in practice, all Victorian self-insurers have adopted the WorkSafe Claims Manual as their baseline for claims management.
72. These principles include that self-insurers must:
- make decisions in accordance with the legislation and follow the procedures in the Claims Manual
- consider all matters relevant to a decision
- not take into account any irrelevant considerations
- exercise discretion when appropriate
- use the best available evidence
- seek out information if it is relevant to the decision, or the information available is inadequate
- give ‘proper, genuine and realistic consideration’ to the merits of a decision
- list all matters considered when making a decision.
73. The Claims Manual also provides guidance to self-insurers on key claims management activities, including:
- determining liability
- following a sound decision-making process
- arranging independent medical examinations and investigations
- processing weekly payments
- terminating weekly and medical payments.
74. WorkSafe’s External Guideline #16 – Claims management policies for self-insurers says that ‘self-insurers must ensure workers are not disadvantaged and will continue to receive at least the same level of entitlement as prescribed in the [Claims] Manual’.
75. Self-insurers also have the option of appointing an agent to manage claims on their behalf. Some companies do this, arguing it provides the best of both worlds for injured workers – the expertise of dedicated claim experts, the industrial knowledge of the employer and streamlined decision-making.
76. Where an agent is appointed, it is the self-insurer's responsibility to ensure that the agent abides by the legislation and the Claims Manual. As the case studies in this report illustrate, poor practice by self-insurer agents can occur when the self-insurer does not fulfill this responsibility.
77. Occupying the position of both employer and insurer creates a significant power imbalance between self-insurers and their workers. This potentially discourages some workers from reporting injuries or making claims.
78. Some self-insurers, like TLC Aged Care, advised they took their role as a self-insurer extremely seriously because of this perceived inequity. Department store operator Myer added that unions can and do play a role in addressing any imbalance. Investigators nevertheless heard accounts of workers who feared for their job if they pursued their compensation entitlements. In some instances, they said that fear was based on what they saw happen to colleagues. Others said they were told directly. Such fears and practices are not limited to self-insurers, but the vulnerabilities of the injured worker are amplified when dealing directly with their employer.
79. The investigation spoke to injured workers of self-insurers who said they were discouraged from or penalised for making a claim. Steel producer BlueScope suggested more claims would be captured by adopting a NSW-style system and placing the onus on self-insurers to proactively contact workers on reporting of an injury to advise of early access to provisional payments and medical treatment.
Resolving claims early
80. There are various ways claims can be resolved early. The investigation was told some methods discourage potential claims from being made.
81. Self-insurers, along with other employers in the WorkSafe scheme, can offer to cover an employee’s medical expenses without the need for a claim. This may meet the worker’s immediate needs and avoid a claims process. As some self-insurers acknowledged, not lodging a claim could leave the worker with limited recourse if their injury or condition did not resolve as anticipated and required ongoing treatment or time off work.
82. Evidence obtained showed that some self-insurers asked injured workers to use their own sick leave instead of putting in a claim. This shifts liability from the employer to the employee, undermining the intent of the workers compensation scheme.
83. The investigation also noted evidence showing some self-insurers offered financial settlements and used internal early intervention programs to resolve claims.
Financial settlements
84. With financial settlements for 'common law damages' often involving long and expensive legal proceedings, there are instances where a self-insurer and workers might prefer to reach an early agreement for a lump-sum payment. The Australian Lawyers Alliance said:
Unlike WorkSafe agents, self-insurers take a proactive approach … and initiate early discussions with injured workers regarding common law damages. These discussions often result in the negotiation of a global settlement which can provide the worker with compensation for their pain and suffering, pecuniary loss and in some circumstances their future medical expenses …
Importantly, it also represents to workers the taking of responsibility by an employer for the occurrence of an injury which serves as an acknowledgement of the harm caused. This early resolution has a positive outcome and benefits the injured worker.
85. Some submissions raised concerns about self-insurers’ use of financial settlements. WIC stated that under the legislation there is only capacity to settle a common law claim for pain and suffering and losses that can be measured in monetary terms. This may not include all possible costs to the injured worker. Submissions consistently raised concern that settlements sometimes followed decisions to terminate entitlements that were not well supported by evidence. It was also suggested workers may be disadvantaged because lump-sum payments were usually conditional on the employer not being held liable for the claimed injury in future proceedings.
86. Self-insurers defended the use of financial settlements. Some claimed workers must be legally represented in certain circumstances. Myer, for example, said a settlement offer that permanently ceases a worker's entitlements under the WIRC Act would require legal representation so the worker can get advice to redress any power imbalance. The WIRC Act does not contain a provision that requires this.
87. Sometimes an injured worker seeks the settlement. Westpac bank told the investigation it was involved in:
numerous cases where the employee is seeking financial settlement, based on independent legal advice and/or advice from their treating medical practitioner, especially where the case involved some psychological distress.
88. When workers are injured, financially vulnerable and possibly in fear of losing their job, a lump-sum payment can appear attractive. Accepting such a settlement could leave the worker without ongoing entitlements and may be to their longer-term detriment.
89. WIC outcomes data shows a large variance in how self-insurer disputes are finalised compared to those of other workers. Between January 2018 and June 2022, WIC issued a genuine dispute certificate due to court proceedings in 16 per cent of self-insurer cases, compared to 0.4 per cent of cases for other workers. This means many more self-insurer disputes were not actively conciliated. These disputes then either proceeded to court or in many cases were finalised prior to court by financial settlement.

90. Often a settlement is conditional on the worker resigning. There may be valid reasons for such a condition, and the worker may have no capacity or desire to return to work. The injured worker may believe their relationship with their employer has broken down. However, pressuring a worker to resign in order to access compensation could amount to a breach of the WIRC Act if it is not legitimate, as the Act is intended to support workers to return to work.
91. Myer stated self-insurers tended to continue the employment of injured workers for extended periods often up to the time the matter was settled, which could be many years after the injury. It submitted the inclusion of a resignation condition was merely a reflection that, at settlement, the employment relationship ceased. This approach does not appear unique to self-insurers.
92. Paying a settlement may be preferred by a self-insurer if it costs less than paying a worker weekly compensation payments and associated expenses long term. This may not be beneficial to the injured worker, and they should have access to all options and understand the risks and benefits to make an informed decision. BlueScope agreed stating ‘it is imperative injured workers be assisted to negotiate in a complex, legalised system’.
93. Anecdotally, it is suggested financial settlements are sometimes made in the absence of a claim. This was not directly examined by the investigation, and the frequency of such settlements is unknown. Given financial settlements are not independently scrutinised, and WorkSafe would have limited jurisdiction over settlements made prior to a claim (unless practices contravened the WIRC Act) this issue warrants further examination to ensure injured workers are protected. It is important settlements made outside of the formal claim process do not contravene the purpose or provisions of the WIRC Act.
94. Case study 1 provides an example of a worker being offered a settlement which if accepted would have disadvantaged the worker by tens of thousands of dollars.
95. Case study 2 provides an example of a self-insurer rejecting a claim to create an avenue for negotiations with the injured worker for a financial settlement. WorkSafe has criticised self-insurers for this practice.
Employer-funded early intervention programs
96. Some self-insurers provide early intervention programs, designed to support staff during the injury management process and improve return to work outcomes. The investigation does not criticise these programs in principle, but we did identify instances where they featured in poor claims management.
97. Each early intervention program is different, but typically includes some form of employer-funded medical services for injury treatment. Some programs provide access to a network of general practitioners, while others have on-site medical and allied health practitioners for timely treatment of minor injuries. Some include support for psychological injuries.
98. Supermarket operator Woolworths launched an early intervention program, including access to clinical specialists and mediation for ‘difficult conversations’ to minimise claim impacts for both the employer and employees. Conglomerate Wesfarmers advised it had adopted a ‘best practice mental health care model’ that:
puts the team members health and wellbeing at the forefront whilst claims management decisions are managed in the background …
[While we recognise] claims for entitlement must be assessed and evaluated rigorously, they need to be balanced with the care owed to team members.
99. Supermarket operator Coles and airline Qantas told us they often prefer to deal directly with workers’ treating practitioners to:
- facilitate timely and ongoing clinical care and rehabilitation
- better understand worker needs
- develop suitable and sustainable return to work options.
100. Self-insurers who provided information about their programs – Qantas, gaming and entertainment group Crown, automobile club RACV, Westpac, Coles, BlueScope, Woolworths and their agent Employers Mutual Ltd (‘EML’) – all emphasised the benefits of early intervention for employees and employers alike. Some focused on the benefits of early access to specialist care including surgery, and many highlighted the importance of compassionate and supportive communication. RACV and Westpac highlighted the contribution of these programs to best practice return-to-work outcomes.
101. Payment of an injured worker’s medical costs and referral to rehabilitation and support services by a self-insurer frequently occurs outside the claims management process because no claim has yet been, or is ever, lodged.
102. Case study 3 provides an example of workplace support and intervention working well.

103. Despite obvious advantages, there are ways in which this model can, by accident or design, produce an unfair outcome.
104. To obtain workers compensation, workers must notify their employer within 30 days of becoming aware of an injury, and must make a claim for weekly payments as soon as practicable. If an injured worker is channelled into an internal rehabilitation program their injury may not resolve as hoped. If they are later denied a claim for this injury based on lodging too late, this is unfair.
105. While some self-insurers accept claims beyond deadlines, the investigation saw several examples of workers’ claims being rejected as ‘out of time’, despite the worker receiving treatment through an internal rehabilitation scheme. Self-insurers should consider all evidence indicating a possible workplace injury irrespective of whether a claim was lodged at that time, as it is reasonable to attempt early interventions without a formal claim.

106. BlueScope advised the investigation early intervention or other programs should not be provided in lieu of a claim being lodged by the injured worker, and that workers must always retain the right to lodge a claim. Myer and Crown agreed and told the investigation their workers are specifically told they retain the right to submit a workers compensation claim after accessing early intervention programs.
107. Case study 5 provides an example of a worker signing away their rights to make a claim when accepting early intervention services. Self-insurers should be wary of asking workers to sign documents that may limit the employee’s rights because as employers they are in an inherently conflicted position to provide advice. Employees should always be provided with accurate information so they can understand their options and give informed consent.
108. While WorkSafe provides WorkCover Assist, a free service to help injured workers with a claims dispute, this is only available when that dispute is referred to WIC for conciliation.
109. In Victoria the early intervention model may in part offset the absence of ‘provisional payments’ for all but mental injuries. The NSW provisional payments system is broader, enabling self-insurers to make weekly payments and cover medical expenses while an injured worker’s claim is assessed.
110. BlueScope advocated for provisional payments to be expanded in Victoria, and stated:
… it negates payment for treatment external to the workers compensation system and captures claims under the legislative framework. The additional cost to insurers would amount to less than 5 per cent of current claim costs and provide certainty for injured workers.
111. It also noted the provisional payment system ‘reduces considerably the wait-time for injured workers to seek treatment’.
Rejecting and terminating claims
112. The investigation found examples of self-insurers rejecting or terminating claims without sufficient evidence to support the decisions.
113. In some instances, self-insurers did not take remedial action when WorkSafe notified them of these problems.
Rejecting claims
114. In 2019, WorkSafe’s Quality Decision Audits found 25 per cent of the rejection decisions audited were not supported by evidence or otherwise unsustainable. It is not clear if these wrong decisions were driven by financial imperatives or were practice or capability issues.
115. In some of the cases, the grounds used to deny a claim did not apply to the worker’s situation. In others, there was simply no evidence to support the decision. The cases where self-insurers maintained these decisions after WorkSafe or WIC told them the decision was contrary to law, demonstrate a need for WorkSafe to be empowered to direct self-insurers to overturn their decisions.
Terminating claims
116. Similarly, investigators saw examples of claims being terminated on unsustainable grounds and self-insurers refusing to overturn their decisions despite advice they were wrong. We also saw positive examples of self-insurers helping injured workers years after they had left the workplace.

Using evidence appropriately
117. Medical evidence and other reports are used both to determine the initial validity of a claim, and to inform ongoing assessments.
118. The Claims Manual requires that self-insurers must:
… take all reasonable steps to seek, obtain and to fairly and properly consider all relevant information before making a decision based on the facts and the merits of the individual case.
119. However, the investigation found examples where self-insurers did not seek appropriate evidence or appear to give it the necessary weight when making decisions.
120. It can be challenging to determine the appropriate weight to give evidence, especially if experts disagree or the right specialist to make an assessment is unclear. All evidence should be examined objectively and not used selectively.
Seeking and assessing the right evidence
121. Some cases reviewed showed self-insurers did not seek sufficient evidence to make an informed decision. This included not seeking or selectively seeking medical reports, vocational assessments to inform job options, or circumstance investigations to determine facts or credibility. These requirements are clear in the Claims Manual, with section 104 of the Act also codifying employer obligations around the return-to-work process.
122. WorkSafe’s Quality Decision Audits showed decisions can be unsustainable because of lack of evidence. In some cases, WorkSafe directly raised concerns with self-insurers that ‘reasonable steps were not taken to seek and obtain relevant information’. In others, WorkSafe found that the available information was not properly considered.
123. In many cases self-insurers disagreed with WorkSafe’s findings, such as these findings from WorkSafe audits conducted between 2019 and 2022:
- The medical evidence does not fully support termination … the psychological secondary is not taken into account at all …
- The decision to terminate weekly payments is based on inadequate evidence and the psychological condition is not assessed at all which makes the decision to terminate [medical expenses] unreasonable. Overall, the decision and evidence gathering is not aligned with WorkSafe’s decision making framework …
- There has been no attempt to assess whether the request is reasonable and necessary … the decision is not supported by evidence and is not appropriate …
124. Case study 7 illustrates how failing to properly obtain, comprehend or give appropriate weight to evidence can lead to poor decisions and detrimental outcomes for injured workers.
125. The importance of obtaining key evidence to inform and support decisions, especially when terminating entitlements, cannot be overstated. BlueScope told the investigation that ‘it would be fairer to say the case studies cited most likely reflect difference of opinion on the collected evidence’. This does not reflect what the investigation found.
126. The investigation examined cases where WorkSafe was critical because workers were not assessed properly: the right specialists were not engaged (eg pain specialists) or there was no expert vocational assessment to identify suitable job options.
127. The case studies demonstrate the need for WorkSafe to be empowered to direct a self-insurer where they have not met their obligations to the injured worker. Active follow-up by WorkSafe is also required where WorkSafe or WIC find that a self-insurer does not understand the law or their obligations to injured workers. The lessons from these case studies should be applied to other claims.
Assessing medical opinions
128. Claims decisions should be based on independent medical opinions. The quality of a medical assessment will be influenced by the quality of the referral seeking it.
129. Investigators were told of ‘doctor shopping’ – instances where self-insurers sought opinions from a variety of IMEs, or only from a preferred IME, seeking an opinion favouring a decision to reject or terminate a claim.
130. Further, it was alleged self-insurers sometimes contacted treating practitioners directly to try to influence the information provided.
131. Given the small number of claims examined in depth by the investigation, this report does not suggest such practices are commonplace. To avoid influencing decisions, or the perception of such, self-insurers should ensure that suitable specialists are engaged, all evidence is carefully considered and that when seeking reviews, claims managers do not deliberately or inadvertently attempt to lead the assessor in a certain direction.
Factual and credibility disputes
132. Various submissions raised concerns about self-insurers focusing on the credibility of the claimant rather than the credibility of the claim, by not properly investigating disputes of fact through circumstance investigations.
133. Claims were also made that self-insurers or their agents sometimes raised factual disputes despite credible medical and other evidence that a workplace injury had occurred. In some cases, this was to reject a claim outright. In other situations, it was alleged this was to circumvent a referral to a Medical Panel.
134. In one case examined, the self-insurer stated the injured worker had ‘credibility issues’ as they had not advised of pre-existing injuries when employed. WIC raised concerns about the self-insurer’s decision to reject the claim in this case, given the actions of the claimant and all the medical evidence (including two IME reports) supported that the injury occurred at work.
Medical Panel opinions
135. The Medical Panel is an expert panel of specialist doctors who come together to resolve medical questions if there is disagreement or uncertainty under workers compensation and personal injury legislation. Referrals to the Medical Panel can be made by WorkSafe and its agents, conciliation and arbitration officers from WIC, and self-insured employers. A Medical Panel cannot be used where there are unresolved factual issues.
136. Section 313(4) of the WIRC Act notes that:
For the purposes of determining any question or matter, the opinion of a Medical Panel on a medical question referred to the Medical Panel—
(a) is to be adopted and applied by any court, body or person; and
(b) must be accepted as final and conclusive by any court, body or person—
irrespective of who referred the medical question to the Medical Panel or when the medical question was referred.
137. Self-insurers most commonly interact with Medical Panels because of WIC referrals. WIC notes that a Medical Panel opinion is final and binding on all parties, and that WIC will issue an outcome certificate which reflects the Medical Panel’s opinion. The opinion may only be challenged in the Supreme Court if a party believes there are errors of law.
138. In some cases, we saw self-insurers following the directions of the Medical Panel as they are supposed to. Case study 9 was submitted by the self-insurer to the investigation as a best practice example.

139. WIC claimed some self-insurers are reluctant to refer to Medical Panels, or create factual disputes as these prevent a referral. This approach to finalising referrals, or refusal to subsequently accept a legally binding opinion, causes delays for injured workers.


Participating in conciliation
140. WIC was designed to provide injured workers and their employers with easy access to free, independent and impartial conciliation and arbitration services. Disputed decisions by WorkSafe agents or self-insurers must go through conciliation at WIC before they can be challenged in court.
141. Binding Ministerial Guidelines in Respect of Conciliation require self-insurers to engage in conciliation meaningfully and genuinely and take all reasonable steps to resolve disputes by:
- providing all relevant information prior to a conciliation conference
- attending the conference
- meaningfully and genuinely discuss all relevant issues raised
- only maintaining decisions which have a reasonable prospect of success, were they to proceed to arbitration or court.
142. Where a dispute cannot be resolved at conciliation, the Conciliation Officer may either certify there is a ‘genuine dispute’ (in which case the dispute may proceed to court) or, if they are satisfied that there is no arguable case for denying payment, give a Direction that weekly payments or medical expenses be paid to the injured worker.
Disputes not resolved
143. The aim of conciliation is to resolve a dispute: this usually means varying the original decision by agreement or recommendation.
144. Self-insurers are over-represented in the number of disputes taken to conciliation. Between January 2018 and June 2022 WIC received 47,663 disputes. Of those, 13 per cent were about the decisions of self-insurers. WorkSafe says that self-insurers account for approximately 6 per cent of new claims lodged annually.
145. Workers of self-insurers are also less likely to get a resolution at conciliation, with WIC data showing fewer self-insurer decisions are voluntarily changed compared to those by WorkSafe agents.
146. Between January 2018 to June 2022 WIC issued 17,334 genuine dispute certificates. Of those, 18 per cent were issued for self-insurer claims.
147. Between January 2018 to June 2022 WIC issued 46 Directions. Of those, 30 per cent were issued to self-insurers.
148. Self-insurers offered reasons other than resistance to conciliation to explain these differences. Crown stated fewer resolutions at conciliation could be because self-insurer decisions ‘are more sound, better informed, and defensible’.
149. Construction supplier Hanson submitted that self-insurers were more likely than WorkSafe agents to make and maintain an adverse decision in a complex matter. Hanson’s view is self-insurers (in contrast to WorkSafe agents) often use one person to manage a case for the life of the claim and this person has detailed knowledge which assists them and leads them to maintain the decision at conciliation, which they believe to be correct.
150. Good administrative decision-making should guide all phases of claims management. Detailed knowledge of a claim should be used, in accordance with the Ministerial Guidelines, to engage meaningfully in conciliation and to take all reasonable steps to resolve disputes. Decision-makers should not be resistant to changing their decisions when the merits of the case warrant.
151. Data reviewed by the investigation shows self-insurers make proportionally more decisions that are disputed, and are less likely to successfully conciliate those disputed decisions.
Adversarial approach
152. Submissions to the investigation spoke about an adversarial and combative approach by some self-insurers at conciliation. People complained of an overly litigious mindset and refusals to alter decisions which had little reasonable prospect of being upheld in court.
153. WIC told the investigation some self-insurers approached claims management and dispute resolution with a litigious mindset, regardless of the merits of the case or the information available. WIC expressed concern these self-insurers seemed to disregard the alternative dispute resolution objectives set out in the WIRC Act. Unsurprisingly, some self-insurers directly objected to these assertions.
154. Some self-insurers said WIC and litigation were necessary avenues for the small number of complex claims which required legal interpretation. They acknowledged concern about some of the problematic conduct by self-insurers reported at WIC, and distanced themselves from such conduct. Some expressed pride in their meaningful engagement and professionalism at conciliation, and called for further examination of conduct issues and for them to be addressed directly with the self-insurers involved.
155. Other self-insurers alluded to problems they experienced with conciliation. One claimed its representatives felt considerable pressure from Conciliation Officers to change its decisions.
156. Another suggested WIC may not have a good understanding of the challenges self-insurers faced at conciliation, so further education may be beneficial.
157. WIC observed self-insurers tend to have the original decision maker as their representative at conciliation. This is supported by Hanson’s observation that the same person who has managed the case is more likely to maintain the adverse decision. This contrasts with the approach taken by WorkSafe agents, where a trained dispute resolution officer will attend, often with ‘fresh eyes’ and potentially more openness to alternative options.
158. WIC stated when decisions or attitudes obstructed an injured worker’s access to a genuine early dispute resolution process this impacted the most vulnerable who were less willing or able to pursue their matter in court.
159. The power and resource imbalance between an injured worker and their employer is obvious, particularly when the employer is a multi-national corporation with access to legal resources. Self-insurers need to be conscious of these dynamics and ensure workers have access to fair and just processes.
160. Some parties observed that law firms representing self-insurers act in a noticeably more aggressive way than those same firms representing WorkSafe agents or WorkSafe directly. Further, WIC raised concerns that firms providing legal advice sometimes provided different advice depending on whether the claim was managed by a self-insurer or a WorkSafe agent, and questioned whether this was because self-insurer decisions had less oversight by WorkSafe.
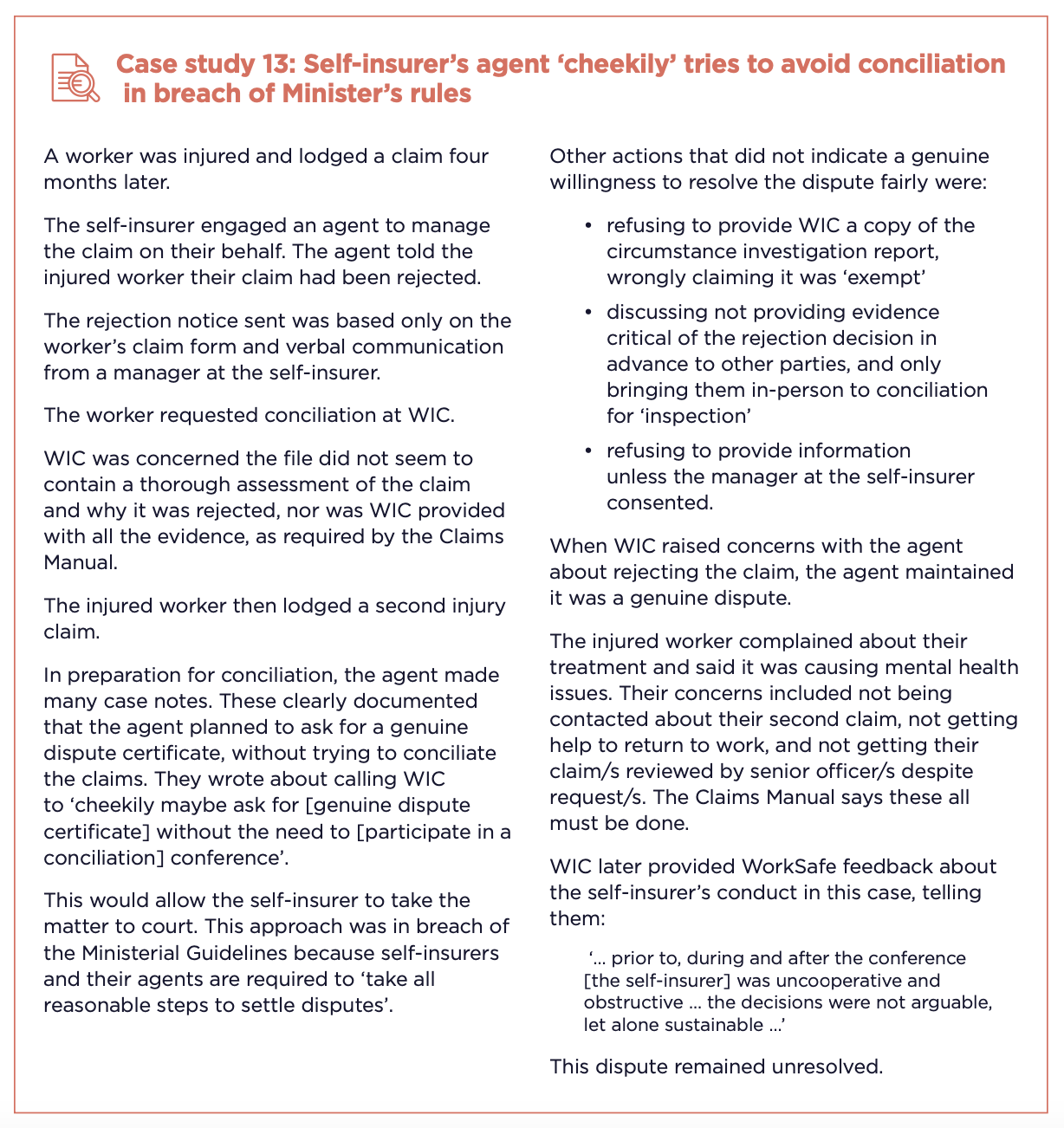
161. The self-insurer’s agent in this case told the investigation claims management issues persisted because the self-insurer had not delegated full decision-making authority to the agent. The agent no longer accepts assignments where its ability to act is limited, to avoid such conflicts.
Following conciliation Directions
162. In very limited circumstances, WIC has the power to direct a self-insurer to make limited weekly payments or limited payment for medical expenses. This can only occur if the conciliator is satisfied that:
- the self-insurer has no arguable case to support the decision in dispute and justify not paying entitlements
- the self-insurer refuses to alter their decision voluntarily.
163. WIC does not issue Directions frequently. They can be appealed to the Magistrates Court. The investigation encountered cases where appeals were unsuccessful, but no formal data is available on appeal outcomes. WIC is not advised if a Direction is overturned. This advice should be obtained and reported on as it would allow assessment of the quality of decision-making by WIC and by self-insurers.
164. Thirty per cent of all Directions issued between 1 January 2018 and 8 June 2022 were to self-insurers. Self-insurers must be open to changing decisions when new evidence is available, or the circumstances warrant a reassessment. This should occur even if it is at the eleventh hour of a conciliation or court case. This demonstrates integrity, accountability and the good administrative decision-making the law requires.
165. The investigation saw cases where self-insurers received advice a decision was unsustainable or received new evidence (including on the day of conciliation) that justified a different decision, yet decisions to reject or terminate were maintained. In some cases, self-insurers were slow to make payments even after WIC directed them to.
166. The failure to comply with a Direction is a breach of the WIRC Act punishable by a $55,000 fine. However, WorkSafe must be aware of the breach for there to be consequences for the self-insurer.
Options when conciliation fails
167. If conciliation fails, injured workers of self-insurers have limited options. One is to withdraw from the process.
168. Another is to seek arbitration. WIC’s relatively new arbitration power allows it to make binding determinations on disputed cases after they have not been resolved by conciliation. This is intended to allow people to resolve claims without having to go to court. Arbitration can only be initiated for injuries that occurred after 1 September 2022. At the end of May 2023, no cases had yet been arbitrated.
169. The final option for workers of self-insurers is to take the matter to court. This option can be stressful and expensive, which is especially challenging for people who are injured and not earning income.
170. Victorian workers who do not work for self-insurers have an extra option available – review by WCIRS. But WCIRS cannot consider cases from self-insurers. Various submissions, including from WIC, raised concerns about this lack of access. WIC said:
… injured workers employed by Self-insurers are further hampered by their inability to escalate decisions for review prior to taking their dispute to court. This clearly disadvantages a worker employed by a Self-insurer and distinguishes them from workers whose employers pay premiums to a WorkSafe Agent …
Workers Compensation Independent Review Service
171. In response to the Ombudsman’s 2019 investigation, WorkSafe established WCIRS in April 2020 to review disputed decisions not resolved at conciliation. WCIRS review officers apply consistent sustainable decision-making criteria to their reviews of claim decisions. They then use WorkSafe’s power in the WIRC Act to give directions to WorkSafe agents to overturn unfair decisions. This part of the Act only applies to WorkSafe agents. No equivalent legislative power exists for self-insurers. Injured workers of self-insurers are therefore currently excluded from access.
Why WCIRS works
172. WorkSafe now has compelling evidence to show the positive impact of WCIRS on decision-making by its agents. A single direction from WCIRS can improve the quality of decision-making for many other claims. WorkSafe agents learn from WCIRS directions and apply the principles to future decisions. This is vital to system improvement. The importance of this within the scheme cannot be understated in WorkSafe’s view. If self-insurers were subject to WCIRS, their decision-making should similarly improve.
173. Over time, if claims managers change to align with WCIRS directions, fewer matters would need to proceed to WCIRS. Figure 5 shows a smaller proportion of WorkSafe agent decisions are being overturned by WCIRS or withdrawn by the WorkSafe agent as the system matures. This is because fewer of the disputed decisions referred to WCIRS need to be changed.
174. The results show in its first months of operation (2019-20), 12 of the 13 disputed decisions referred for review (92 per cent) were overturned by the Review Officer or withdrawn by WorkSafe agents. Many more disputed decisions were referred for review the following year (301) with the proportion overturned or withdrawn still relatively high at 50 per cent. In the 2021-22 financial year, only 38 per cent of decisions referred for review were overturned or withdrawn.
175. This process is an important oversight mechanism for WorkSafe that delivers meaningful and systemic improvement.

176. Self-insurers account for a disproportionate number of disputes at conciliation and Directions issued by WIC. Given this, WCIRS may act as an equally strong (if not stronger) impetus for change in self-insurer practices than already seen among WorkSafe agents.
177. This would require close collaboration between self-insurers and momentum by WorkSafe to drive change and develop best practice.
178. It is also noted that only four WorkSafe agents in Victoria manage claims for about 95 per cent of the work force, making it relatively easy for these agents to apply learning from one wrong decision to many other claims. This may be much harder for the 34 self-insurers, some of whom deal with only a small number of claims.
What self-insurers say
179. While some self-insurers acknowledged the current inequity in access to WCIRS, few directly supported the need for change to close the gap; their responses to the draft report instead calling for more detail on how change could be implemented and operationalised.
180. In its response to the draft report, healthcare company Healius claimed that WCIRS reviews were limited in scope in that they only look at adverse decisions:
There has not been any review of decisions made to accept liability which should have been rejected … quality of decision making goes both ways …
It may well be … that the reduced number of disputes being raised with respect to [WorkSafe] Agents is an outcome of [WorkSafe] Agents accepting claims because this is the most practical solution in the circumstances.
181. Westpac did not support self-insurers being subject to WCIRS, stating the conduct of a few should not be considered reflective of all. Crown maintained only self-insurers who engaged in poor conduct should be subject to WCIRS.
182. BlueScope presented a mixed view. It agreed all injured workers should have the right to access WCIRS, though stated in their experience:
WorkSafe are no better positioned to interpret complex matters than an insurer, and ultimately a matter may need to be determined in a legal forum.
183. In their responses to the draft report Westpac, Wesfarmers, Crown, Hanson and RACV called for more detail about how the power to direct by WorkSafe would be implemented and called for review mechanisms to apply.
184. Agent EML which currently acts for three self-insurers, welcomed the suggestion that WCIRS be extended to include self-insured employers to further ensure fair and equitable outcomes for all injured workers. Wesfarmers was also broadly supportive and advised it saw no reason for the employees under a self-insurance program to be subjected to different rights and processes. It suggested a trial of any new process should be considered to assess the effect on claims experiences and conduct.
185. These varied responses indicate the purpose and current functioning of WCIRS may not be well understood. It is not a punitive measure. Fixing the current inequity of WCIRS access would only have an impact on self-insurers who made unsustainable decisions. There would be no basis to overturn decisions of self-insurers undertaking claims management in line with best practice and the legislation.
WorkSafe oversight
186. One of WorkSafe’s key functions is to oversee self-insurers to ensure they manage claims in accordance with laws designed to protect workers and support their return to work. WorkSafe is responsible for approving and monitoring self-insurers to enforce performance standards and promote good decision-making.
187. WorkSafe is also responsible for ensuring self-insurers comply with the Charter of Rights Act. Denying and terminating genuine claims is unfair. Not only could it result in the employees being financially disadvantaged, it could also lead to a loss of dignity and self-esteem and reputation within the workplace.
188. WorkSafe believes that the principles underlying the Claims Manual align with the Charter of Rights Act, however, we saw no evidence that WorkSafe comments on workers' human rights when reviewing claims decisions. Wesfarmers was the only self-insurer to make specific mention of human rights in its response, telling the investigation the company understands and embraces its obligations under the Charter of Rights Act and that corporate values of integrity, accountability and openness underpin their approach to management of its self-insurance portfolio.
189. WIC noted workers of self-insurers are particularly vulnerable and raised questions about WorkSafe’s oversight:
The shortcomings that these [earlier] reports consistently identified with WorkSafe’s oversight of [its] agents are further compounded in the context of Self-insurers, due to the limits of WorkSafe’s role as regulator.
190. While WorkSafe does not have the same power over self-insurers as it does over WorkSafe agents, it is not powerless. It took steps to improve system oversight following our 2016 and 2019 investigations.
191. WorkSafe made further changes in March 2023 to obtain more timely and comprehensive data about claims and decisions, so it is not intervening months later. WorkSafe is also analysing data to identify issues early so it can work with self-insurers, peak bodies, conciliators and agents to remedy poor practice and improve systems.
192. Despite these initiatives, WorkSafe appears to struggle to effectively regulate self-insurers in some areas, constrained in part by the limits of its legislative powers.
193. This report has already highlighted an instance where WorkSafe has failed to verify or scrutinise implementation of its Quality Decision Audit recommendation to the self-insurer. This may have allowed poor practices to continue. WorkSafe acknowledged that verification of Quality Decision Audit recommendations had not been undertaken consistently.
194. During our investigation, WorkSafe acknowledged that a change of approach was required. WorkSafe implemented a procedure to verify the outcome of all its Quality Decision Audits with self-insurers who have agreed with its recommendations. This new procedure ensures the agreed changes are actioned.
195. Another limitation is WorkSafe’s inability under the WIRC Act to direct a self-insurer to overturn an unsustainable decision. In several of the case studies in this report, self-insurers said they agreed with WorkSafe’s recommendations but then did not follow them. WorkSafe’s position as regulator and subject matter expert did not convince those self-insurers to change their decisions.
196. For WorkSafe to compel a self-insurer to change a decision that is unsustainable, it needs this legal power. WorkSafe has not taken any steps to seek this power. It argued it is just now seeing the impact of the power to direct WorkSafe agents as they change their practices in response to WorkSafe’s directions.
197. WorkSafe told the investigation it would welcome the power to direct self-insurers to overturn an unsustainable decision.
198. The power to review and overturn self-insurers’ decisions is not unprecedented in Australia. In Queensland, for example, the Office of Industrial Relations conducts independent reviews which can confirm, vary or set aside a self-insurer’s decision. These are based only on the application and claim file, and review officers cannot make enquiries or conduct investigations.
Approving self-insurers
Initial approval
199. An employer applying to be a self-insurer must first demonstrate to WorkSafe that it is ‘eligible’ under section 375 of the WIRC Act. This primarily means showing it is capable of meeting its potential claims liabilities.
200. Self-insurers must also demonstrate they are ‘fit and proper’. In addition to the employer’s financial viability, WorkSafe must look at a self-insurer’s:
- safety record
- number of workplace injuries
- cost of associated claims
- capacity to manage claims.
201. When assessing the company’s resources for managing claims, WorkSafe advises prospective self-insurers it expects:
a strong claims management, occupational rehabilitation and return to work history, including compliance with the [WIRC Act], appropriate participation and implementation of agreements in conciliation processes, strong results in worker satisfaction surveys, and minimal substantiated complaints, which have been resolved in a timely manner if they occur.
202. In other jurisdictions, expectations of self-insurers are articulated in a more detailed way. For example, in South Australia approval as a self-insurer is conditional on the self-insurer abiding by a detailed Code of Conduct.
203. Finally, WorkSafe must also have regard to ‘such other matters as the Authority thinks fit’. This provision means WorkSafe can consider any other relevant topic. WorkSafe has used this provision to request details of prosecutions under the WIRC Act and details of an employer’s consultations with their employees and relevant unions about the proposal to become a self-insurer.
204. The names of organisations applying to be self-insurers are posted on WorkSafe’s website, and anybody with relevant information can make a submission to WorkSafe as part of the initial approval process.
205. If approved, the new self-insurer is granted an initial approval period of three years.
206. After this, self-insurers may apply to WorkSafe for reapproval. The standard reapproval term is four years. The reapproval process is WorkSafe’s key mechanism for managing self-insurers’ performance and is designed to be informed by data from its various monitoring systems. Reapproval of self-insurers is discussed more later.
Outsourcing to agents
207. The WIRC Act allows a self-insurer to ‘appoint a person approved by the Authority to act as the self-insurer’s agent’ to carry out the role.
208. In 2023, eight self-insurers have WorkSafe approval to outsource the management of some or all of their claims to agents.
209. In a submission, one of these agents, EML, identified its perception of the benefits of ‘effectively managed self-insurance’ as:
- providing immediate access to care and support
- ensuring continuity of care for workers
- bringing strong workplace knowledge, allowing them to tailor and establish suitable duties to assist with an early and sustainable return to work
- delivering direct feedback on opportunities to change operational processes to improve safety and prevent injuries.
210. EML provided its perspective on the advantages of self-insurers using ‘specialist claims managers’. For example, it suggested specialist claims management brings a higher level of expertise and understanding of regulatory requirements.
211. EML also said it provided independent decision-making, though noted in the past not all self-insurers had delegated them full decision-making power. EML acknowledged this had led to conflicts in decision-making.
212. In response to the draft report EML noted that the current Ombudsman investigation had identified opportunities for improvement. It advised it had made significant improvements to its services to self-insurers following the Ombudsman’s previous WorkSafe investigations. EML told the investigation it had:
observed the positive impact of these changes on our decision making including achieving 100% compliance in the most recent WorkSafe Quality Decision audits undertaken in April and November 2022.
213. In contrast, BlueScope questioned whether self-insurer agents offered superior decision-making to self-insurers, noting the conduct of [WorkSafe] agents had led to a review of claims management practices initially by the Ombudsman and other oversight bodies or regulators. Hanson also recommended caution weighing the perceived benefits of appointing an agent. This report includes case studies highlighting problematic approaches involving both self-insurers and their agents.
214. Ordinarily, WorkSafe can direct its agent to overturn a decision. As noted, WorkSafe cannot do this when the agent is acting on behalf of a self-insurer. Perhaps not surprisingly, several submissions raised concerns that agents can behave differently when acting for self-insurers.
215. EML emphasised separate business units manage self-insurer claims and other workers compensation claims. While such separation may be appropriate for management purposes, it carries a risk that any positive changes may not flow equally across the whole system. If changes are made to one claim because the approach or decision was wrong, they should apply to all subsequent claims, no matter the type.
Monitoring self-insurer performance
216. WorkSafe monitors self-insurers through a combination of audits, feedback and complaints. This framework is designed to ensure self-insurers meet their statutory obligations. It adopts a targeted approach for oversight and intervention in line with the risk profile of individual self-insurers.
217. WorkSafe’s oversight framework includes multiple monitoring mechanisms:
- Claims Management Audits
- the tier system
- Self-insurer Self-audit Program
- Performance Improvement Plans
- regulatory monitoring (including complaints, WIC lodgements, enforcement activity and the comprehensive review of performance in the lead up to reapproval).
218. WorkSafe also receives information about self-insurer performance through:
- Quality Decision Audits
- health checks
- injured worker surveys.
219. WorkSafe reports back to self-insurers on monitoring activity via quarterly reports (about complaints, WIC lodgements and enforcement activity) and a yearly Self-Insurer Performance Snapshot (‘yearly report’).
220. WorkSafe says yearly reports 'contain insights into a self-insurer’s performance across key areas of being “fit and proper”, including safety, services to injured workers, and financial and prudential capacity’. These reports are sent to self-insurers for the attention of the CEO or equivalent (such is their importance) and include ‘areas of interest and/or areas of concern that require improvement’. WorkSafe does not follow up to ensure the self-insurer understood the issues highlighted or acted on required improvements.
Claims Management Audits
221. In the year before a self-insurer’s approval term expires, WorkSafe conducts a Claims Management Audit. This checks performance against a set of claims management criteria, although none of these criteria evaluate decision-making quality.
222. The self-insurer's performance against the audited criteria is expressed as an overall ‘compliance rate’, out of a possible 100 per cent. This rating is used to place self-insurers into different ‘tiers’.
The tier system
223. The tier system, introduced in 2018, is fundamental to WorkSafe’s risk-based approach to oversight – focusing less on those self-insurers who are performing well. How much monitoring and reporting a self-insurer is subject to depends on their performance (see Figure 6).

224. While Tier 1 is only for self-insurers rated 95 per cent and higher, Tier 2 covers a large range. A high-performing self-insurer with a compliance rating of 94 per cent can be categorised and monitored the same as one with only 80 per cent. Currently, no Victorian self-insurer is rated Tier 3.
225. Unlike NSW, self-insurers' tiers are not published in Victoria. Publication of performance and assessment information enhances transparency and accountability across the sector and may motivate self-insurers to improve their performance.
226. At present, Victorians have no way of knowing which self-insurers are performing well. The compliance ratings and tiers for WorkSafe-approved self-insurers at the time of this report’s publication are shown in Appendix 3. Because tier assessments for self-insurers are not reviewed by WorkSafe each year the assessments for some self-insurers are several years old.
227. Of the 34 self-insurers operating in Victoria, 17 are rated Tier 1, and 16 are Tier 2. One, multinational resources company BHP, is not rated because it has not had auditable activity. In such cases, WorkSafe reattempts the audit every subsequent year until there are claims to audit.
228. Several self-insurers’ compliance ratings do not match their assigned tier as there is a significant lag between WorkSafe calculating a rating and assigning a tier at reapproval. For example, food company Mondelez achieved only 71 per cent compliance in 2022 which ought to place them in Tier 3 but it remains in Tier. Mondelez is not due to be assigned a new tier until reapproval in November 2023.
229. Mondelez told the investigation this compliance result made for sobering reading. Mondelez advised it had reflected on the poor audit result and engaged experts to improve performance. The self-insurer’s commitment to improving its performance is commendable. WorkSafe should consider what it can do to address flaws in the tier system itself.
230. The tier determines the number of audits the self-insurer must undergo during its approval term. A Tier 1 self-insurer will be audited three times during a six-year approval period, while a Tier 2 self-insurer would usually be audited four times during that period.
231. A self-insurer’s tier also influences the circumstances in which improvement plans are required by WorkSafe. These plans are completed by self-insurers to address performance issues identified in audits. Tier 1 self-insurers are allowed a 10 per cent decline in compliance rating before an improvement plan is required, while a Tier 2 self-insurer is allowed only a 5 per cent decline.
232. It is in a self-insurer’s best interest to be in a higher tier, and WorkSafe states the main purpose of the tier system is to encourage performance improvement. However, there are flaws with the system.
233. Tier placement is based solely on the Claims Management Audit in the year before a self-insurer’s approval term expires, which does not evaluate decision-making quality. Other data and feedback available to WorkSafe about self-insurer performance does not affect tier ratings. This needs more consideration from WorkSafe.
234. Also, a self-insurer's tier does not change throughout its approval term. Irrespective of how its performance may change, the level of oversight remains consistent for up to six years.
235. In contrast, NSW regulator State Insurance Regulatory Authority (‘SIRA’) takes a more holistic approach, and reviews self-insurers’ tiers at least annually. A self-insurer’s conduct, claims management practices and financial viability are all used to determine their tier. SIRA contemplates shortening licence periods for poor performers. SIRA reserves Tier 1 for ‘exemplar performance’ only.
236. WorkSafe’s approach is different. Sometimes WorkSafe uses its discretion to assign self-insurers to a higher tier, even when their compliance rating is below the minimum for that tier. WorkSafe’s guideline to self-insurers about oversight explains:
If a self-insurer’s compliance rate is borderline below achieving a Tier 1 or Tier 2 level of compliance, WorkSafe may apply a margin of 3% and assign the self-insurer to the higher tier level, taking into consideration the:
- action required to rectify their non-compliances
- overall performance under the measures listed under regulatory monitoring in the framework.
237. It is unclear why this discretion is applied at all, and only to assign a self-insurer to a higher tier. This may create a ‘near enough is good enough’ approach to compliance, rather than self-insurers having a clear consequence if they do not meet the required benchmark.
Self-audit Program
238. Self-insurers are required to audit themselves through the Self-insurer Self-audit Program (‘self-audit’). The self-audit contains two aspects. Part I relates to occupational health and safety and Part II relates to claims management, employer obligations and other requirements. This investigation has only considered Part II of the self-audit.
239. Like the Claims Management Audit, the frequency of self-audits required depends on the self-insurer’s tier and approval term. Tier 1 self-insurers must complete a self-audit twice during any approval term; Tier 2 must self-audit three times.
240. Self-audits are undertaken by an external auditor nominated by the self-insurer who WorkSafe mandates must have ‘suitable qualifications, knowledge and experience’. WorkSafe provides detailed instructions on the criteria and sampling methodology. The criteria used mirror the Claims Management Audits, so self-audits also do not examine the quality of a self-insurers' decision-making.
241. Self-audits lead to an overall compliance rate expressed as a percentage. These ratings do not influence the self-insurer's tier as the Claims Management Audits do. The average rating over the financial years 2018-19 to 2021-22 varied markedly for each self-insurer, with one as low as 67 per cent, while others averaged 100 per cent.
242. Where a self-insurer fails to meet certain requirements, it must prepare a remedial action plan to correct deficient practices. WorkSafe monitors remedial action plans required due to non-compliance at self-audit.
243. WorkSafe states it uses the self-audits to:
- monitor and promote continuous improvement in claims management and return to work practice
- include in the yearly report
- identify breaches of the WIRC Act, which WorkSafe may investigate.
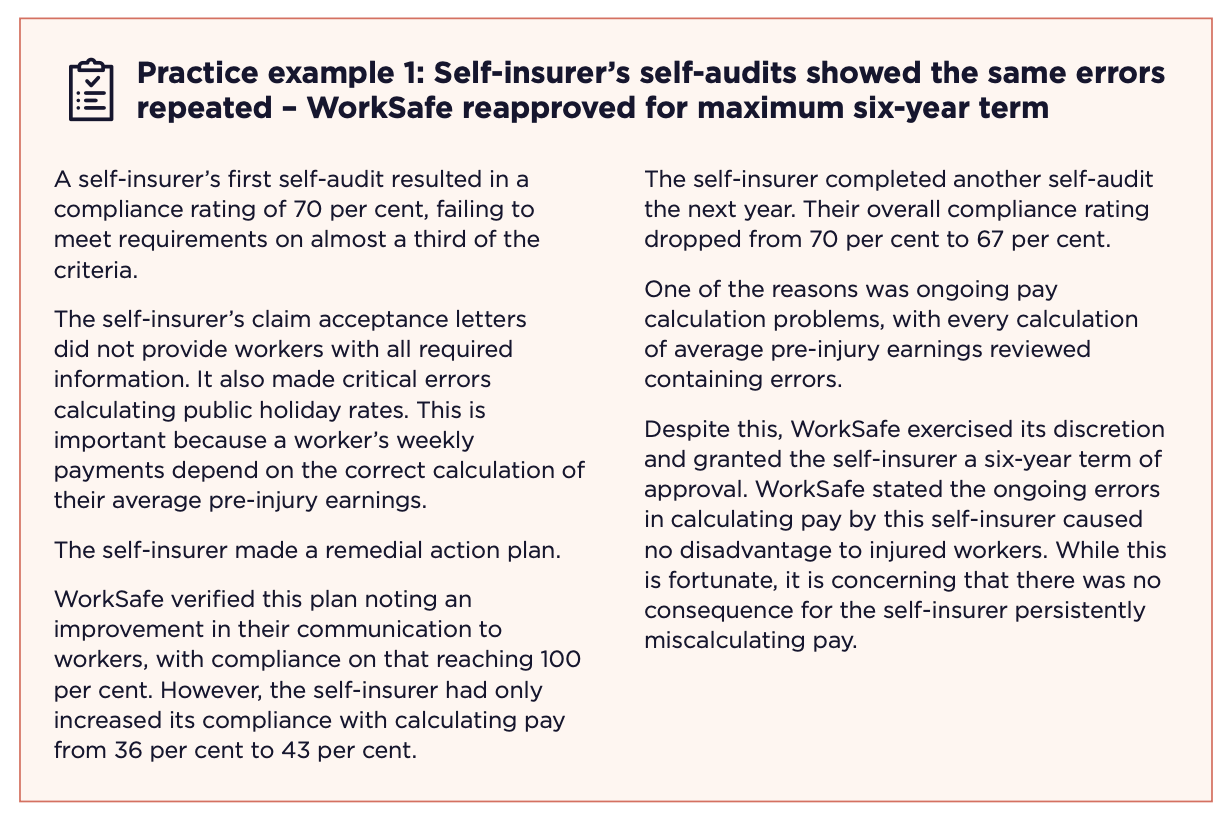
244. WorkSafe advises auditors who conduct self-audits that remedial plans must be prepared and reported ‘for criteria that did not meet requirements which are indicative of systemic deficiencies in practices’. Systemic deficiencies include:
- incorrect interpretations of legislative requirements
- incorrect application of WorkSafe’s policies
- repeat findings that financially impact a worker’s entitlement, like the miscalculation of average pre-injury earnings
- repeat findings which require a review of remedial actions.
245. Auditors are told that 'an effective remedial action will correct a deficient practice and prevent future recurrences’. As illustrated in Practice example 1, more needs to be done to verify if remedial plans are effective and this must influence WorkSafe’s assessment of the competence of the self-insurer, including when determining reapproval and terms.
246. WorkSafe has mechanisms for addressing repeated non-conformance. It can revoke a self-insurer’s approval or impose additional obligations. We discuss WorkSafe’s use of these mechanisms in the section on managing poor performance by self-insurers. To be effective, these mechanisms need to be used, and be seen to be used.
247. As well as highlighting issues with individual self-insurers, self-audit results can be a useful comparison with WorkSafe’s Claims Management Audits. The investigation compared self-audits from 2019 to 2022, against the most recent WorkSafe Claims Management Audit and found variances in the compliance ratings.
248. Although most self-insurers’ self-audit ratings are broadly consistent with their Claims Management Audit ratings, where there was a substantial variation, the better result was achieved in the Claims Management Audit. This supports information provided to the investigation suggesting some self-insurers devote significant resources to performing well in Claims Management Audits. This may be because this determines their tier.
249. We also found a self-insurer’s tier is not necessarily representative of how they will perform over the life of their approval period because compliance ratings can change significantly. The average self-audit compliance rating for Tier 1 self-insurers was around 94 per cent, which is below the Tier 1 benchmark.
250. One self-insurer had a 24 percentage point drop in Claims Management Audit compliance during its six-year approval term. However, it remained at Tier 1 even though this did not accurately reflect its current performance. This self-insurer’s own self-audits showed a steady performance decline but there was no change to the oversight regime by WorkSafe based on the tier. Earlier intervention may have prevented the decline and had a necessary and positive impact on the injured workers whose claims were being managed.
251. WorkSafe should link the outcomes of self-audits to the tier determinations and ensure when issues are identified, prompt remedial action is taken.
Quality Decision Audits
252. WorkSafe audits a sample of self-insurer’s claim decisions every year to confirm alignment with WorkSafe’s sustainable decision-making framework. We refer to these as ‘Quality Decision Audits’ in this report. WorkSafe and self-insurers often call these ‘Quality Decision-Making Audits’ or ‘QDMs’.
253. These reviews specifically aim to ensure decisions:
- are supported by reasonable, appropriate and sufficient evidence
- afford injured workers procedural fairness in assessing entitlements
- have not wrongfully disentitled injured workers
- are communicated accurately, clearly and in a timely manner.
254. WorkSafe assesses whether each decision meets the quality criteria for initial claims liability, medical expenses and entitlements to weekly compensation. The findings in past reviews can influence the focus of future reviews. For example, in 2019-20 WorkSafe audited ‘initial eligibility’ decisions and found almost 25 per cent did not meet the criteria. Having identified this as an area of concern, it audited more cases where this type of decision was in dispute the following year.
255. This is a good example of a targeted and responsive approach, because WorkSafe’s focus appears to have had a significant impact on the practices of self-insurers. In 2020-21, 95 per cent of audited ‘initial eligibility’ decisions passed.
256. WorkSafe assesses decision-making compliance based on good administrative decision-making principles, which are set out in the WorkSafe Claims Manual. These principles are underpinned by the Quality Ethical Decision-making framework detailed in the manual.
257. This approach was developed and implemented in response to recommendations made in our second workers compensation investigation in 2019. This approach is also consistent with the tests applied by WCIRS in deciding if a decision is sustainable.
258. Before 2019, WorkSafe did not conduct Quality Decision Audits of self-insurers. From 2019 to 2022 WorkSafe completed 575 reviews of individual decisions of self-insurers, of which 57 failed one or more requirements.
259. Results varied a lot between self-insurers. Some performed very well, failing few, if any, audit criteria. The results of Quality Decision Audits are not made public by WorkSafe. Several self-insurers advised the investigation their most recent Quality Decision Audits showed 100 per cent compliance. The Ombudsman encourages each self-insurer to make their Quality Decision Audit results, and all other audit results, public.
260. Quality Decision Audit failures from 2019 to 2021 did not align with the self-insurers market share. For example, one self-insurer that employs less than 3 per cent of the self-insurer workforce in Victoria accounted for 16 per cent of the Quality Decision Audit fails. Others with similar market share had no audit failures.
261. Only in 2022 did WorkSafe start considering Quality Decision Audit results as part of its reapproval assessment. WorkSafe told the investigation this three-year lead time was required to ‘establish procedures, benchmarks and to provide procedural fairness to self-insurers’.
262. Many of the issues WorkSafe identified in Quality Decision Audits appeared to be recurring and there is no evidence WorkSafe intervened or adequately followed-up after it notified self-insurers’ of key audit fails. For example, the investigation found two of the largest self-insurers received feedback they had failed to take reasonable steps to obtain relevant and available information before making decisions. This is a significant issue that should have attracted close follow-up from WorkSafe.
263. When a self-insurer fails a Quality Decision Audit, WorkSafe makes recommendations to the self-insurer. However, this does not guarantee the decision will be revisited. This is because WorkSafe does not possess the power to direct self-insurers to overturn their decisions when its recommendations are ignored.
264. While Quality Decision Audits are useful for providing information about self-insurers decision-making practices, they are not an effective mechanism for changing self-insurers' decisions or improving practices. WorkSafe believe that Quality Decision Audits did result in some self-insurer decisions being changed and some overall improvements. Nevertheless, it described the use of Quality Decision Audits without legislative authority to require a self-insurer to change a decision as ‘a lost opportunity’.
265. In several cases examined, self-insurers disagreed with WorkSafe’s finding that a decision was unsustainable. WorkSafe provided the investigation its analysis of the Quality Decision Audits. This showed 55 cases where self-insurers expressly disagreed with WorkSafe.
266. Self-insurer rejections of WorkSafe’s assessment were often based on:
- a misunderstanding of the Claims Manual or the right process
- a failure to consider whether the decision was sustainable.
267. In only three cases self-insurers advised WorkSafe of changed decisions.
268. In other cases, the self-insurer failed to provide any response to WorkSafe. WorkSafe also did not enquire about whether any wrong decisions were changed.
269. WorkSafe said it was committed to taking a more active role in verification of outcomes where the self-insurer agreed the decision was not sustainable. Where the self-insurer did not agree, WorkSafe believed it could not take further steps.
270. WorkSafe advised the investigation that:
… neither the legislation nor the Ministerial Order allow [WorkSafe] to direct the self-insurer to accept a claim for compensation or to reinstate benefits to an injured worker if the decision does not meet WorkSafe’s requirements.
271. As such, WorkSafe considers it is limited in the extent to which it can intervene in a claim outcome, even where, in their opinion as the system’s regulator, they find a decision to be incorrect or unsustainable.
272. WorkSafe tries to make an impact on self-insurers’ decisions by making recommendations – for example, recommending they seek further IME reports, seek further non-medical evidence or simply they change their decision. However, in most cases WorkSafe does not know what happens after it completes its audits.
273. One issue is that the WorkSafe team conducting the audits does not have access to the relevant claim file once the Quality Decision Audit has been finalised.
274. Second, WorkSafe in the past has not followed up with the self-insurer to determine whether its recommendations on individual claims have been implemented. In February 2023, WorkSafe advised the investigation it would implement a new practice of verifying whether the self-insurer had implemented the recommendations. However, it would only do this on claims where the self-insurer agreed with WorkSafe’s findings. WorkSafe stated it did not consider it had the power to take any action where a self-insurer disagrees. So, this new approach is still limited.
275. WorkSafe is also improving the timeliness of Quality Decision Audits for self-insurers. Audits currently occur up to six months after the decision. At that stage, some decisions have already been the subject of conciliation and been ruled a genuine dispute. WorkSafe explained as time passes and disputes escalate, it is harder to get a self-insurer to change their position.
276. Case study 14 demonstrates a self-insurer not giving appropriate weight to a medical opinion. Despite WorkSafe finding the self-insurer and their agent were wrong, and that the decision to reject the claim was unsustainable, no action was taken when the self-insurer disagreed.

277. Case study 15 provides another example of where the decision of a self-insurer, and their agent, was wrong. Even though the self-insurer’s agent agreed with WorkSafe’s Quality Decision Audit finding flaws in the decision, it was not changed.

278. While WorkSafe does not have the power to direct self-insurers, it does have the power to consider self-insurer’s claim management performance as part of its renewals process. At this time it also considers the occupational health and safety performance and the financial sustainability of the self-insurer.
279. Quality Decision Audits are a useful source of data for WorkSafe in this regard, as the claims are audited in detail by WorkSafe’s own claims specialists. This material has been used in only a few renewal processes since 2022.
Health checks
280. WorkSafe’s ‘health checks’ are used to monitor the introduction of new legislative requirements or when a theme emerges from audits or other oversight activities.
281. Health checks are conducted ad-hoc across both parts of the scheme – WorkSafe agents and self-insurers. In 2021 for example WorkSafe conducted a health check to look at IMEs who had been engaged by, or on behalf of, a self-insurer in the past year. WorkSafe did so as they had received information that self-insurers and their agents were using non-approved doctors to complete IME reports.
282. WorkSafe found more than one in 20 medical examinations it reviewed were conducted using a non-approved IME. WorkSafe reminded self-insurers and their agents such reports would be invalid under the WIRC Act.
283. WorkSafe has continued to monitor this without further issues being identified.
284. This demonstrates health checks can be an effective mechanism for change, when regulatory activity identifies an emerging issue.
Injured worker surveys
285. WorkSafe actively seeks feedback from injured workers. Every year it surveys a selection of workers on an array of topics including overall satisfaction, communication, independent medical examinations, health and wellbeing and returning to work. The surveys cover both WorkSafe agents and self-insurers and result in individual and aggregate ‘all [WorkSafe] agent’ or ‘all self-insurer’ scores.
286. Some self-insurers have very few claims. WorkSafe considers the minimum number of respondents required for a meaningful survey result is 20. Self-insurers with fewer claims do not receive individual results, but their claims are included in aggregate scores.
287. WorkSafe considers 75 per cent a strong satisfaction score. Historically, self-insurers’ scores have remained around 10 per cent lower than the ‘all agents’ score. ‘All agents’ scores ranged from 71–74 per cent between 2019 and 2022. ‘All Self-insurer’ scores during the same period ranged from 62-64 per cent.
288. Survey data showed many self-insurers’ average scores below 75 per cent in the past seven years. Only one with a score of 76.5 per cent exceeded the average satisfaction level of the ‘all agents’ score across this period.
289. There is scope for self-insurers to influence the result of surveys. Self-insurers are asked to identify any claimants who should be legitimately excluded on the grounds they have threatened to harm themself or others, or because of current litigation.
290. Figure 7 shows an email chain in which a claims staff member from a self-insurer’s agent asks a senior manager for a worker to be excluded from the survey because they complained to a Government Minister. The self-insurer agent’s spreadsheet to WorkSafe said the reason was ‘Risk of harm to self. Notable behaviour’.
291. Figure 8 shows the response from another of the self-insurer agent’s claims officers seeking all injured workers whose claims they had rejected or terminated be excluded from the satisfaction survey. In the end, the self-insurer agent did not ask WorkSafe to exclude the four workers from the survey because agent management did not consider the email request from the claims officer when finalising the list of workers to exclude.
292. In response to the draft report, the self-insurer agent said extra emails it held provided further context. The agent submitted that under time pressure to get the information to WorkSafe, the manager providing the list did not wait for staff input or consider the requests by staff referenced in these emails. The manager simply excluded all injured workers with flags on the self-insurer agent’s system identifying them as at risk of harm, having known aggressive or threatening behaviours, or ‘do not contact’ requests. This raises questions about how injured workers are excluded from satisfaction surveys, and WorkSafe’s oversight of this process.
293. WorkSafe told the investigation it ultimately excluded ‘a handful’ of the 68 workers the self-insurer agent requested be excluded but did not provide further details of why. The emails and the attempts to remove injured workers from the survey list by the self-insurer agent staff indicate WorkSafe needs to do more to ensure lists are validated and exclusions are necessary.
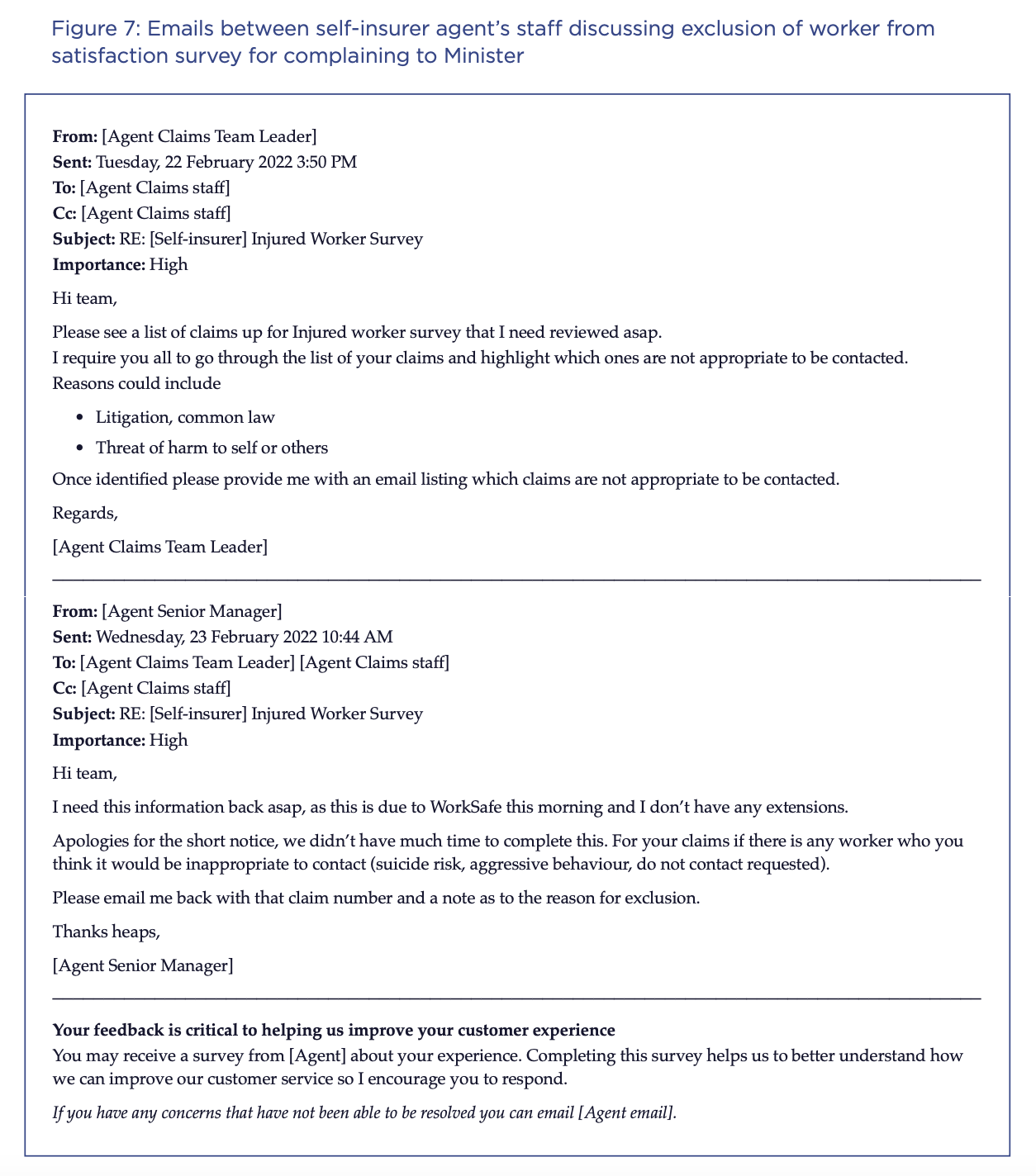


294. WorkSafe’s staff discuss the survey results with self-insurers and include them in yearly reports. WorkSafe added that:
… where the results for an individual self-insurer are markedly different to a previous survey result … [WorkSafe] may request the self-insurer provide an explanation and a remedial plan to address the survey result.
295. Practice example 2 shows an instance where WorkSafe acted following a drop in satisfaction among a self-insurer’s injured workers. While WorkSafe took some action, its subsequent lack of follow-up allowed problems to continue without effective intervention for years.

296. In addition to the informal discussions and communications WorkSafe has with self-insurers about their results, the surveys are meant to inform the reapproval process.
297. WorkSafe’s guidelines note when assessing for being ‘fit and proper’ it will generally consider the survey results for ‘service score’ and ‘overall prompted satisfaction’. It is also required to consider ‘any programs the self-insurer has put in place to address the overall satisfaction of injured workers’.
298. In Practice example 2, the downward trend and below-par scores of the self-insurer did not seem to influence the reapproval decision. WorkSafe needs to address this issue.
Complaints
299. At any point in the claims process, an injured worker can complain to WorkSafe about the management of their claim. This complaint process was centralised and better resourced following the Ombudsman’s 2019 investigation.
300. WorkSafe has created detailed specific guidance material for its complaints staff for complaints about self-insurers.
301. WorkSafe received 169 complaints – an average of about 65 per year – about self-insurers between 1 December 2019 and 30 May 2022.
302. We compared self-insurers’ percentage of complaints to their share of the self-insurance market to see if they were over-represented in complaints. As with Quality Decision Audits, complaint numbers for most self-insurers did not align with market share. For some self-insurers complaint numbers were much higher and for others much lower than expected. Eleven self-insurers drew no complaints.
303. Complaint numbers are not always a good representation of performance, or worker satisfaction. For example, some injured workers may be discouraged from complaining to WorkSafe or the Ombudsman, while other self-insurers may actively promote these options. Accordingly, WorkSafe must do more to interrogate this data alongside other sources of information such as surveys, health checks and audits to form a comprehensive view of where problems lie and where to target its resources.
304. BlueScope told the investigation that, given the number of claims self-insurers would have received during this period, it could be concluded most claimants were satisfied with their experience.
305. Our analysis showed of the 169 complaints, 34 were substantiated by WorkSafe, either partially or in full.
306. The substantiated complaints related to 13 self-insurers, 11 of whom are still currently approved as self-insurers.
307. WorkSafe told us that when complaints are substantiated:
- WorkSafe notifies the self-insurer
- the complaint forms part of the self-insurer’s performance assessment documented in an annual report card to each self-insurer
- the complaint is considered as part of the approval renewal process.
308. We reviewed three recent yearly reports for self-insurers with substantiated complaints and found in five cases WorkSafe failed to mention them. The CEO receiving their annual report card should be provided with this essential information.
309. Positively, we also saw evidence that WorkSafe acts promptly to assess complaints, draws them to the attention of the self-insurer, and seeks a practical resolution.
310. WorkSafe’s External Guideline #3: Assessment of application for renewal of approval as a self-insurer notes that:
WorkSafe will generally consider the following information and indicators for being fit and proper:
- The number and nature of complaints
- Whether or not complaints have been substantiated
- Whether there are recurring themes in complaints
- Whether there are any issues or trends arising from complaints.
311. In practice, complaints may have little impact on reapproval. Practice example 3 shows how complaints about a self-insurer were identified but the maximum term for reapproval was granted anyway.

WIC Feedback
312. WIC is well placed to provide information about issues with self-insurer’s claims management practices.
313. This aligns with WorkSafe’s External Guideline #3 – Assessment of application for renewal of approval as a self-insurer which says that as part of renewal applications they will consider self-insurer conduct at conciliation including:
- timely and proper participation and cooperation with WIC
- Prompt implementation of conciliation agreements and directives
- any other issues raised by WIC.
314. WorkSafe told the investigation that they speak with WIC staff regularly and are always open to feedback. It acknowledged that it only formally seeks WIC’s feedback on self-insurer conduct at the time of renewal of approval. Only formally requesting information at the renewal stage is problematic and this is another lost opportunity for WorkSafe, especially if the self-insurer is approved for a six-year term.
315. The investigation found an example where WIC was concerned about issues with a self-insurer’s conduct at a conciliation held in June 2021, yet WorkSafe did not become aware until 20 months later when they sought feedback as a part of approval renewal.
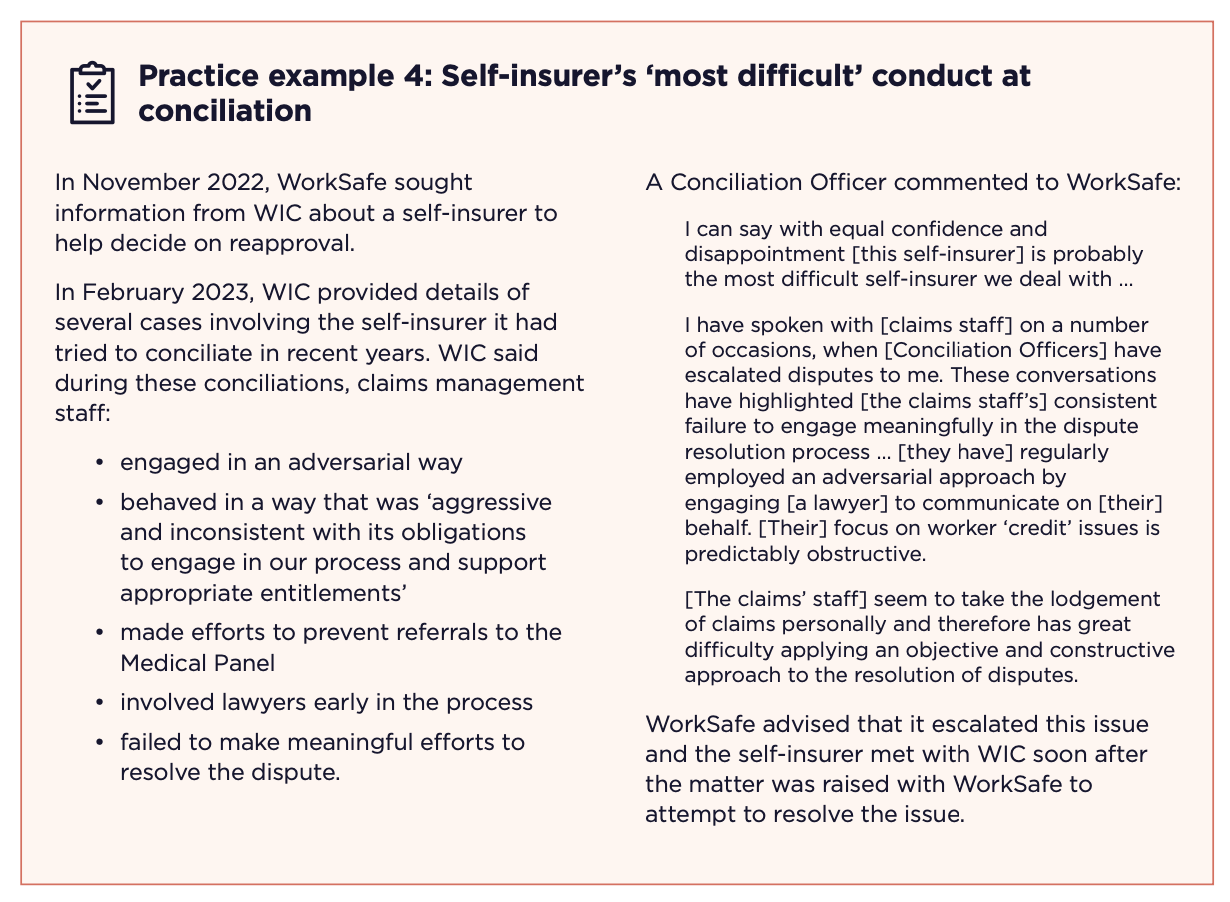
316. It is concerning that WorkSafe was not aware of this serious criticism for such a long time.
317. WIC can offer feedback on its own initiative, although in practice they consider this to conflict, to a degree, with their independent role. WIC suggested that although WorkSafe is receptive to feedback, the regulator was perhaps at times unable to act because of the limitations of its oversight powers.
318. WorkSafe acknowledged if WIC raised concerns of repeated issues with a self-insurer, WIC would be advised to raise this directly with the self-insurer.
319. As the regulator, WorkSafe should ensure systems are in place for WIC to notify it of performance and conduct concerns at conciliation. Self-insurers must then be informed of serious issues promptly to give them the opportunity to address concerns. WorkSafe has specific obligations to ensure self-insurers are ‘fit and proper’ throughout the life of their approvals.
Reapproving self-insurers
320. At the end of their initial term of approval, self-insurers apply for reapproval. WorkSafe must be satisfied that they continue to be ‘fit and proper'.
321. WorkSafe tells self-insurers they must:
- have appropriate resources in place to ensure high performance in administering claims
- conform with WorkSafe’s audit standards
- have a strong history in claims management, occupational rehabilitation and return to work
- comply with the WIRC Act
- participate appropriately in conciliation
- have strong results in worker satisfaction surveys
- have few substantiated complaints, which should be resolved in a timely manner.
322. The reapproval process is a significant oversight mechanism. The list above indicates most of the monitoring activities conducted by WorkSafe will be factored into its reapproval decision. WorkSafe tells self-insurers it expects them to demonstrate a high standard and continuous improvement. This instruction needs to be matched by a firm regulatory approach by WorkSafe when the evidence shows otherwise.
323. WorkSafe told the investigation it undertakes a comprehensive assessment of whether a self-insurer remains ‘fit and proper’. However, not all the information WorkSafe collects through its monitoring activities is considered.
324. WorkSafe’s ‘comprehensive assessment’ at reapproval did not consider the quality of self-insurer decision-making on claims until 2022, despite WorkSafe collecting detailed information about this since 2019. Quality Decision Audit fails indicate problems ranging from poor communication with injured workers, to repeated breaches of the Claims Manual and the WIRC Act.
325. WorkSafe also has a useful source of information in self-insurers’ responses to its negative Quality Decision Audit findings. While self-insurers do not always respond, the nature and tone of received responses ought to be considered more by WorkSafe during the reapproval process, particularly where they demonstrate limited understanding of sustainable decision-making.
326. WorkSafe is also meant to consider whether self-insurers genuinely engage in conciliation. We found no evidence of a strong regulatory response when self-insurers, their agents or their legal teams, behave in a way that is contrary to the guidelines or intentions of conciliation.
327. In Case study 13, where a self-insurer agent tried to get a genuine dispute declared without having to conciliate, WorkSafe reviewed the case and found the self-insurer had:
… [a] reluctance … to attend face-to-face conferences at conciliation due to resource issues … and at conciliation … they were [noted by WIC to be] uncooperative, obstructive and failed to provide material in a timely manner.
328. Despite this, WorkSafe found the self-insurer was 'fit and proper’. WorkSafe decided the poor attitude to conciliation and other performance issues could be addressed by placing a condition on the reapproval. In this instance the self-insurer was reapproved for a standard four-year term, but we also saw self-insurers with poor performance granted six-year terms.
329. WorkSafe has stated they reapprove self-insurers with performance issues as they do not wish to take a ‘punitive approach’. They want to collaborate with and educate self-insurers to improve practices. While this can be constructive, some of the case studies in this report raise the question of just how bad a self-insurer’s conduct needs to be before their approval is reviewed, made conditional or revoked.
Discretion to approve for six years instead of four
330. At the time of reapproval, WorkSafe also decides the length of the new term. The standard term is four years, but WorkSafe can approve a term of six years. The investigation was troubled by WorkSafe’s tendency to use its discretion to approve six-year terms for self-insurers with claims management performance issues.
331. There are advantages to securing a six-year term and self-insurers would understandably prefer it. Both the reapproval process itself and the audit regime are less frequent.
332. The six-year term should be reserved for consistently high performing self-insurers with a proven track record of best practice.
333. However, WorkSafe’s guideline for reapproval states:
In applying its discretion to grant a self-insurer an approval for a six-year period, WorkSafe will consider the self-insurer’s performance against indicative performance benchmarks. A self-insurer may be recommended for a six-year period of approval, even if all the indicative performance benchmarks have not been met.

334. The investigation saw other examples of WorkSafe approving six-year terms for self-insurers that were not strong performers.
335. A couple of years ago, WorkSafe audited a self-insurer prior to its renewal. The self-insurer received a compliance rating at the bottom of Tier 2 for its Claims Management Audit. They received some poor results in key areas – less than 10 per cent compliance for accurately calculating pay rates and about 30 per cent for providing injured workers with all appropriate information.
336. WorkSafe assessed the self-insurer as having sufficient resources to manage claims and being ‘fit and proper’. The self-insurer only met two of the four benchmarks relevant to it for consideration of a six-year term. It partially met a third and failed to meet the fourth. Nevertheless, WorkSafe granted a six-year term.
337. WorkSafe places a great deal of faith in the good intentions of self-insurers even when it sometimes has information to the contrary. As detailed in Case study 16, WorkSafe started prosecuting a self-insurer for repeated case management failures and alleged breaches of the WIRC Act. When giving the self-insurer notice of its reapproval, WorkSafe explained the decision to grant the maximum six years was in part because it believed the self-insurer would not commit further offences.
338. If the discretion to give a six-year term instead of the standard four is exercised so often that it is now actually the exception for a self-insurer to be granted a standard four-year term, then WorkSafe’s risk-based approach to regulation needs revision. Their approach ought to be based on only the top performers being approved for the maximum term, not this being the standard. Otherwise the effectiveness of discretion and the usefulness of one of the few levers available to WorkSafe to encourage improvement is undermined.
Managing poor performance by self-insurers
339. There are two main mechanisms WorkSafe can use to regulate self-insurers outside of the reapproval process: section 384 reviews which can lead to approval being revoked, and enforcement actions.
‘Fit and proper’ review under section 384 of the WIRC Act
340. WorkSafe has the power to review the approval of a self-insurer ‘at any time’. If it is ‘no longer satisfied’ that the self-insurer is ‘fit and proper’ it must conduct a review under section 384 of the WIRC Act.
341. Other situations which trigger a review are set out in section 384 of the WIRC Act, including when self-insurers experience liquidity problems, or are subject to merger, acquisition, restructure, or foreign ownership.
342. These reviews are broad in scope. WorkSafe can use existing performance reports, audits, and consultations with external bodies to verify relevant information. In some cases, WorkSafe may convene a panel of senior staff to consider the material obtained and hear submissions from stakeholders before making recommendations.
343. After the review, WorkSafe can impose conditions on the self-insurer or revoke their approval if no longer satisfied that the self-insurer is ‘fit and proper’.
344. In practice, revocation of a self-insurer's approval under the WIRC Act has never been pursued because of a self-insurer’s claims management practices. WorkSafe said:
To the best of our knowledge, there is no evidence that WorkSafe made a decision to terminate/revoke a self-insurer or not re-approve a self-insurer due to issues with claims management in the last twenty years.
345. This is despite WorkSafe identifying repeated issues in claims management with some self-insurers, including errors calculating entitlements appropriately, poor conduct at conciliation, decisions not made in accordance with the WIRC Act and failures to comply with Directions as highlighted in the case studies.
346. WorkSafe has only conducted one section 384 review due to claims management practices.

347. In Practice example 6, WorkSafe could have constructed conditions that required meaningful and measurable changes to the self-insurer’s practice at conciliation to manage the risk to injured workers. WorkSafe did not do this, a lost opportunity.
348. The ability to impose conditions on self-insurers is a powerful tool. Many of the issues highlighted in the case studies throughout this report could usefully have been subject to a formal review.
Enforcement action
349. As a last resort, WorkSafe can take enforcement action to prosecute self-insurers alleged to have committed offences under the WIRC Act. In practice this happens very rarely.
350. When deciding whether to prosecute and what enforcement action should be taken, WorkSafe considers the sufficiency of the evidence and the public interest, in accordance with its General Prosecution Guidelines and its Compliance and Enforcement Policy.
351. Prosecutions of self-insurers who commit offences under the WIRC Act can attract a financial penalty, and some carry possible prison terms.
352. According to its prosecution guidelines, WorkSafe is targeting ‘offences by employers that unduly delay a worker’s access to entitlements, for example, failing to make weekly payments and ‘breaches by self-insurers'.

353. As shown in Case study 16, WorkSafe may accept a written undertaking given by a self-insurer for breaches of the WIRC Act, excluding the most serious offences, such as those which carry a term of imprisonment. The prosecution is then discontinued.
354. When weighing whether to prosecute, WorkSafe is required to consider the public interest. It should take into account the nature and circumstances of the offending and the characteristics of the offender. WorkSafe should also give regard to its own guidelines for prosecution and consider ‘the extent to which the alleged offender has acted in accordance with any advice given by WorkSafe in relation to its obligations’.
355. The public interest test reasonably includes considering whether prosecution would act as a specific deterrent to the self-insurer, and a general deterrent to other self-insurers.
Conclusions
356. This investigation was quite targeted in scope and focused on a relatively small number of self-insurer cases. Overall, some self-insurers are performing well and delivering the benefits the system intends, such as immediate and continuous care informed by knowledge of the workplace. However, the cases we examined in detail exposed large differences in practice and capability.
357. The current claims management process and oversight of self-insurers does not always produce fair or equitable outcomes for workers.
358. Injured workers, advocates and sector experts told us that financial settlements, early intervention programs and dispute resolution processes can all be misused. Despite clear feedback from WIC about the failure by some identified self-insurers to engage meaningfully at conciliation, the current regulatory regime is not able to stamp out this conduct. Injured worker surveys and complaints can also be distorted and have a diminished value if they are not accessible to all workers and do not result in action from WorkSafe to address recurring and serious issues.
359. Our case studies highlight examples where self-insurers can learn from poor outcomes, as well as positive practices that show what can be achieved with the right approach. Most self-insurers and their agents acknowledged the case studies identify opportunities to improve claims outcomes or practices.
360. Some self-insurers told the investigation that WorkSafe operates constructively and collaboratively and implements a strong regulatory program for self-insurance that includes various assurance processes across data, claims and disputes. The investigation found WorkSafe could do more in its role as regulator of self-insurers. While WorkSafe's level of responsibility differs for self-insurers compared to the WorkSafe agent model, they are nevertheless ultimately responsible for ensuring that self-insurers comply with legislation and act with integrity to protect injured workers.
361. Despite having robust powers, expertise and performance-monitoring systems, WorkSafe has not acted swiftly or in a sufficiently targeted way to address some issues with self-insurers who do the wrong thing. It seems WorkSafe has been reluctant to use its existing compliance mechanisms to enforce performance standards. In some cases, WorkSafe has not followed up to confirm the implementation of its own recommendations about decisions which did not comply with the WIRC Act. There are instances where WorkSafe reapproved self-insurers, often for longer than standard terms, without resolving performance issues. It also does not define best-practice claims management.
362. There are some flaws with WorkSafe’s default position of education and collaboration with self-insurers. This position works well when self-insurers align their approach to workers compensation with their obligations under the legislation, and they have the insight and capability to change. However, this approach should be balanced with punitive measures to enforce standards when required, sending the message that poor performance will not be tolerated, and that the regulator is watching.
363. There are many regulatory tools available to WorkSafe that could be used more effectively, not least the review and reapprovals processes. The investigation found too often WorkSafe approved self-insurers for the maximum six-year term without evidence of exemplary performance to justify these decisions. In some cases, there were known compliance issues with these self-insurers. If others see there are no consequences for poor performance, a poor ethical climate can fester.
364. WorkSafe should be empowered to direct self-insurers, as it does its agents, to overturn decisions that are unsustainable or wrong. Without this direction power, WorkSafe is ultimately hamstrung as a regulator if self-insurers or their agents ignore their recommendations or advice. This can force injured workers, who may have no income and be seriously unwell, into contesting their rights in court.
365. WorkSafe presented compelling arguments for having a direction power. It would address a fundamental gap which is limiting the rights and outcomes for injured workers of self-insurers in Victoria. While WorkSafe has reportedly had internal discussions about the issue, disappointingly, it appears not to have taken any meaningful steps to urge amendment to the legislation despite sound public policy reasons for doing so.
366. Improvements and positive changes have been made to the workers compensation system since our first investigation of WorkSafe agents’ practices in 2016. WIC’s new arbitration power is one, but this is yet to be tested. WorkSafe’s use of its ability (through WCIRS) to direct its agents to change an unsustainable decision has led to a system-wide uplift in practice.
367. It is unclear how much change self-insurers have embraced voluntarily given they were not the focus of past investigations, and WorkSafe’s different regulatory approach. Some self-insurers consider the current arrangements with WorkSafe are reasonable and claim a proven track record of collaboration with WorkSafe.
368. The evidence gathered in this investigation suggests that the current arrangements do not produce consistent, quality outcomes for injured workers. Where there are gaps, it is important that WorkSafe has the power to direct self-insurers in the way it can with its agents.
369. It is clear WorkSafe needs to conduct a comprehensive review of all self-insurers, and this should include how they engage with WorkSafe. The issues identified in this report may not apply to all self-insurers, and there may be other practices that warrant attention because they do not support or protect injured workers as intended by the legislation.
370. WorkSafe has a central role and under-used potential as a transformative leader and regulator for self-insurers. The investigation identified opportunities to ensure WorkSafe supports self-insurers to understand and implement best practice; lifts benchmarking; and makes quality assurance and public accountability a priority.
371. Until all workers in Victoria who have the right to claim workers compensation also have the same rights when they disagree with a decision, the system will remain fundamentally unfair. Self-insurers say they want independence to offer more to their valued employees. The proof of these intentions is evident every time an injured worker makes a claim.
372. Some workplace injuries are catastrophic. Some people are never able to work again. So, when a worker is having their worst day at work, self-insurers need to bring their best. In the public interest, all Victorian workers deserve the protection of a fair, equitable and accountable statutory compensation scheme.
Responses to the investigation
373. While 22 self-insurers did not offer a substantial response to the investigation’s draft report, those who did demonstrated an openness to making continuous improvements.

374. Some self-insurers were displeased with the Ombudsman’s decision to withhold the names of self-insurers involved in case studies and practice examples. They were not themselves the subject of these examples and wanted the Ombudsman to make this clear in her report. This was not possible as it had the potential to identify the injured workers in the case studies. The Ombudsman is committed to transparency and recommends WorkSafe make public performance information for all self-insurers.
375. Two self-insurers opposed legislative and practice changes enabling WorkSafe to have the power to direct a self-insurer to change unsustainable decisions.
376. Healius argued the power was unnecessary. It stated the draft report showed ‘no evidence of widespread inappropriate behaviour by self-insurers’ so tools already at WorkSafe’s disposal such as education, auditing and conditions on approvals were adequate, and that arbitration needs to ‘be given time to work’. Healius said directing a self-insurer would be ‘inappropriate’ in situations where the self-insurer had legal opinion that the grounds for rejecting liability were defendable in court.
377. BlueScope also objected, claiming no other Australian workers compensation scheme regulator was empowered to direct a self-insurer’s decision-making. BlueScope stated such an approach was ‘at odds with the fundamental principle of direct ownership of claims decisions and cost borne by self-insurers’. Further, it said WorkSafe were ‘no better positioned to interpret complex matters than an insurer, and ultimately a matter may need to be determined in a legal forum’.
378. In saying this, BlueScope agreed injured workers should have access to WCIRS, the team in WorkSafe that reviews disputed decisions of WorkSafe agents and can direct them to overturn a decision. BlueScope also made a commitment to ‘improving the experience and outcomes for injured workers’. It acknowledged the complexity of workers compensation and that the ‘sometimes-difficult task of recovery should not be impeded by poor claims management’.
379. WorkSafe committed to implementing the recommendations directed to it in this report. WorkSafe believes that it has demonstrated a commitment to improving its oversight of self-insurers. However, it acknowledges that when claims management fails there is an impact upon workers, families and workplaces. While the majority of claims managed by self-insurers meet regulatory and community expectations, WorkSafe stated that it remains resolved to address the issues identified in this report.
380. The Minister for WorkSafe and the TAC responded to the investigation’s draft report. The Minister acknowledged the impact inappropriate claims management can have on injured workers and their families and supported the intent of the recommendation to the government to review the WIRC Act. The Minister identified this recommendation is:
designed to improve regulatory oversight of self-insurers and result in fair and equitable outcomes for injured workers that are employed by self-insurers.
381. The Minister stated WorkSafe is fulfilling its obligations in relation to its regulatory oversight of self-insurers, especially in financial liability. Nevertheless, the Minister indicated a willingness to review approval and oversight arrangements in other Australian jurisdictions to identify improvements. The Minister also noted the significant impact WCIRS has had on the quality of WorkSafe agent decisions and promised to:
work with WorkSafe to explore the potential to extend this mechanism, and its underlying operating principles, to the self-insurance context.
Opinion
382. As part of its key functions, WorkSafe must ensure self-insurers deliver claims management in accordance with laws designed to protect workers and support them to return to work. WorkSafe is responsible for approving and monitoring self-insurers, developing and enforcing performance standards and promoting good decision-making under the WIRC Act, including acting compatibly with human rights under the Charter of Rights Act.
383. Pursuant to section 23(1)(g) of the Ombudsman Act, the Ombudsman is of the opinion that the actions of WorkSafe in relation to regulation and oversight of self-insurers were wrong in that WorkSafe did not take adequate action to oversee or otherwise regulate self-insurers to promote compliance and performance.
384. This is relevant to cases highlighted in this investigation where WorkSafe was or should have been aware that a self-insurer’s, or their agent’s, decisions or conduct were contrary to law, the Claims Manual or WorkSafe guidelines, including its sustainable decision-making framework.
Recommendations
Pursuant to section 23(2) of the Ombudsman Act, the Ombudsman recommends the following actions.
To improve regulatory oversight of self-insurers
It is recommended that the Victorian Government and the relevant Minister:
Recommendation 1
Review the Workplace Injury Rehabilitation and Compensation Act 2013 (Vic) and related Ministerial Orders to:
a. empower WorkSafe to independently review disputed decisions when requested by injured workers of self-insurers following unsuccessful conciliation, and overturn decisions that do not have a reasonable prospect of success at court
b. ensure that compliance mechanisms available to WorkSafe more adequately respond to non-compliance by self-insurers.
The review should include consideration of effective options such as mandatory codes of conduct and approval processes used in other jurisdictions.
To improve the experience and outcomes for injured workers
It is recommended that WorkSafe:
Recommendation 2
Conduct a review of all self-insurers' claims management practices to ensure they align with legislative requirements and the conduct expected of public authorities.
Recommendation 3
Make use of the information collected through audits, injured worker surveys, complaints and other available sources, to better inform the approval and reapproval of self-insurers, including the term of the approval.
To promote better transparency and accountability of self-insurers
It is recommended that WorkSafe:
Recommendation 4
Publish information about self-insurers including:
a. approval conditions
b. tier ratings and approval terms
c. claims management performance information such as injured worker survey results and audit outcomes
d. significant compliance and enforcement activity.
Appendix 1: The investigation
Authority to investigate
385. Under the Ombudsman Act 1973 (Vic) the Ombudsman’s jurisdiction extends to investigating administrative action taken by or in an authority, and whether an administrative action is incompatible with a human right set out in the Charter of Rights and Responsibilities Act 2006 (Vic).
386. This investigation was conducted under section 16A of the Ombudsman Act, which provides the Ombudsman may conduct an own motion investigation into any administrative action taken by or in an authority.
387. Being a public statutory body as defined in the Ombudsman Act, WorkSafe is an authority within the Ombudsman’s jurisdiction. As specified entities under item 18 of Schedule 1 to the Act, self-insurers are also authorities subject to the Ombudsman’s jurisdiction.
What the investigation involved
388. On 27 May 2022, the Ombudsman notified the relevant Minister, Chief Executive Officer of WorkSafe, Chair of WorkSafe’s Board of Directors and the Chief Executive Officer of the Accident Compensation Conciliation Service (now WIC) of her intention to investigate this matter.
389. Between 27 and 30 May 2022, the Ombudsman notified the Principal Officer of each current Victorian self-insurer of her intention to investigate this matter.
390. The investigation involved:
- Reviewing legislation, including:
- Workplace Injury and Rehabilitation and Compensation Act 2013 (Vic)
- Accident Compensation Act 1985 (Vic)
- Charter of Human Rights and Responsibilities Act 2006 (Vic)
- Ministerial Order – Terms and Conditions of Approval as a Self-Insurer (April 2016)
- Ministerial Guidelines in Respect of Conciliation (August 2022).
- Reviewing 6,695 pages of WorkSafe’s documents, policies and procedures, including:
- WorkSafe Claims Manual
- WorkSafe Claims Management Audit – Information pack 2022
- External Guidelines:
- #2 – Assessment of initial application for approval as a self-insurer
- #3 – Assessment of application for renewal of approval as a self-insurer
- #4 – Application for approval of a person to act as an agent of a self-insurer
- #6 – Self-insurer Self-audit program 2021-2022
- #11A – Self-insurance oversight framework for claims management
- #14 – Resources for managing claims
- #16 – Claims management policies for self-insurers
- #19 – Review of self-insurer’s approval
- WorkSafe Complaints Management Policy
- Sustainable Decision-Making Reference Guide.
- Reviewing other WorkSafe documents, including:
- Self-insurer Performance Snapshots (SIPS)
- Quality Decision Making Audits (Quality Decision Audits)
- Claims Management Audits.
- Engaging with the Workplace Injury Commission (WIC), and obtaining and reviewing WIC documents and data, including:
- conciliation files
- reports
- emails
- annual reports.
- Receiving information from various sources (including submissions) regarding about 240 potential claim files.
- Issuing summonses to 12 self-insurers and one self-insurer agent to produce selected claim files, claims management data and emails of selected staff; reviewing the summonsed material.
- There were 867,998 items obtained, including:
- 87 individual claim files
- 165,420 emails
- 48,509 documents
- 8,613 Excel spreadsheets
- Receiving and considering written submissions from 45 parties, including:
- 20 injured workers, or family members and advocates
- Workplace Injury Commission
- Victorian Trades Hall Council
- Australian Manufacturing Workers Union
- Australian Workers’ Union
- Transport Workers’ Union of Australia
- Shop, Distributive and Allied Employees’ Association
- Australian Nursing and Midwifery Federation
- Flight Attendants’ Association of Australia
- Australian Lawyers’ Alliance
- Australian Services Union
- Law Institute of Victoria
- United Workers Union
- Health care providers
- Self-Insurance Association of Victoria
- BlueScope Steel Ltd
- Coles Group Ltd
- Crown Resorts Ltd
- CSR Ltd
- Qantas Airways Ltd
- Royal Automobile Club of Victoria (RACV) Ltd
- Viva Energy Group Ltd
- Healthy Working Lives Research Group, School of Public Health and Preventive Medicine, Monash University
- Employees Mutual Ltd.
Appendix 2: List of current self-insurers
Figure 10: List of Victorian self-insurers, March 2023
- Alcoa of Australia Limited
Amcor Ltd
BHP Group Limited (‘BHP’)
BlueScope Steel Ltd (‘BlueScope’)
BP Australia Group Pty Ltd
Brambles Ltd
Brickworks Ltd
Carter Holt Harvey Building Products Pty Ltd
Coles Group Ltd (‘Coles’)
CSR Ltd
ExxonMobil Australia Pty Ltd
Food Investments Pty Ltd (‘Food Investments’)
Hanson Australia (Holdings) Pty Ltd (‘Hanson’)
Healius Ltd (formerly Primary Health Care Ltd) (‘Healius’)
Inghams Group Ltd
Liberty Holdings Australia Ltd
Mars Wrigley Australia Holdings Pty Ltd
Melbourne Water Corporation
Mondelez Australia Holdings Pty Ltd (‘Mondelez’)
Myer Holdings Ltd (‘Myer’)
Paper Australia Pty Ltd (‘Paper Australia’)
Philip Morris (Australia) Ltd
Qantas Airways Ltd (‘Qantas’)
Robert Bosch (Australia) Pty Ltd
Royal Automobile Club of Victoria (RACV) Ltd (‘RACV’)
SS Silver Pty Ltd (formerly Crown Resorts Ltd) (‘Crown’)
TLC Aged Care Pty Ltd (‘TLC Aged Care’)
Toll Holdings Ltd
Toyota Motor Corporation Australia Ltd
University of Melbourne
Viva Energy Group Ltd (‘Viva Energy’)
Wesfarmers Ltd (‘Wesfarmers’)
Westpac Banking Corporation (‘Westpac’)
Woolworths Group Ltd (‘Woolworths’)
Source: Victorian Ombudsman
Appendix 3: WorkSafe compliance ratings of self-insurers
Figure 11: Compliance ratings of self-insurers (by WorkSafe Tier) at 14 December 2022


Appendix 4: Improvements made in response to the Ombudsman’s prior investigations
Figure 12: Improvements to the oversight of self-insurers made since 2019

